
Achalasia and cancer prevention and surveillance
Introduction
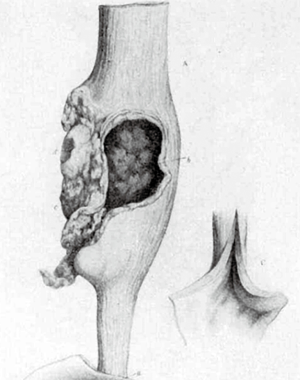
The association between achalasia and esophageal cancer (EC) has long been recognized. The first description of this association occurred in 1872, when an English physician called Charles Hilton Fagge described a case of an 84-year-old patient with a 40-year history of dysphagia, who developed a tumor in a dilated portion of the esophagus (Figure 1) (1). Since then, several studies have shown this association (2-5).
Several putative factors are identified as causative for this association, from chemical irritation caused by saliva and food decomposition in esophageal lumen secondary to stasis could lead to dysplasia (6); increased volatile nitrosamines secondary to bacterial growth inside the esophagus (7) to genetic factors (8).
Achalasia and cancer risk
The real chance of a patient with achalasia developing esophageal squamous cell carcinoma (SCC) is unknown and it is variable in the literature. Absolutely discrepant rates have been described ranging from 0 to 33% (9-14). In a paper that reviewed clinical studies with a minimum follow-up of 5 years, Eckardt et al. found rates closer to reality, ranging 0 to 7% (15).
Although some older studies have not shown cases of esophageal cancer in patients with achalasia (9,16,17), two recent meta-analysis have shown that the incidence rate of SCC in patients with achalasia varies from 1.36/1,000 patients-years (18) to 3.12/1,000 patients-years (19) and express risks, respectively, of 1.5% and 2.8%. These rates are 15 and 34 times higher, respectively, than the risk of esophageal SCC in the general population, according to the International Agency for Research on Cancer (IARC) (20). Furthermore, these studies have shown that the onset of cancer rarely occurs before 5 years of disease, and after the tenth year that the incidence increases significantly. Another meta-analyses found an incidence rate of 2.05/1,000 patients-years in patients treated for achalasia, especially after 10 years of disease (21). Thus, according with the Guidelines of the International Society of Diseases of the Esophagus (ISDE), patients with achalasia have a moderate increase in the risk of developing CCS within 10 years of initial achalasia treatment (22).
There is evidence that patients with achalasia have an increased incidence of esophageal adenocarcinoma (EAC) up to 6 times higher than the general population (19) and this fact could be explained by the carcinogenic effect of treatment of achalasia leading to gastroesophageal reflux disease (GERD) and Barrett´s Esophagus (BE) (23,24). Indeed, BE has been reported up to 9% after achalasia treatment with pneumatic dilatation (25) and in 5.5% after Per Oral Endoscopic Myotomy (POEM) (26). BE after Heller myotomy and fundoplication (HMF) is a rare event and appears long time after treatment and it dependent on failure of the operation (27,28). However, there are cases of EB development in untreated patients (29). The reason for this phenomenon is unknown, and the main hypothesis is that chronic inflammation caused by food and saliva retention could trigger the cascade of events leading to BE (30). However, the real association between achalasia and EAC is controversial and remains unknown.
This variation of risk, prevalence and incidence rates is probably explained by duration of follow-up of achalasia in each study (11,19,21), since significant increase in the onset of neoplasia is observed in long-term studies (15).
Surveillance and prevention
The role of surveillance in achalasia is a topic that has been discussed for decades with no consensus and several controversies (30-32). Patients with achalasia have a higher relative risk than the general population to developing EC (10 to 50 times), but with a relatively low absolute risk (about 1.5% to 3%). These rates express an incidence of 0.1% to 0.3% per year (18,19). It means that we need to perform about 400 endoscopies in patients with achalasia to find 1 case of EC (11). Besides that, there are conflicting data about the efficacy on early diagnosis and prognosis of EC in this population (10,14,15). This perception that endoscopic surveillance may not affect the prognosis of the neoplasia (10,33) makes it harder to homogenize a management and create surveillance guidelines de. Indeed, important societies such as the ISDE (22), the American Society of Gastrointestinal Endoscopy (ASGE) (34) and the American College of Gastroenterology (ACG) (35) do not recommend specific routine surveillance in these patients, only consider the possibility of endoscopy from 10 to 15 years of disease. Similar recommendations can be found in recent papers (15,36,37).
On the other hand, a risk of 0.3/year is comparable to the risk of Barrett esophageal malignancy without dysplasia (38) or low-grade dysplasia (39) and in these specific situation the surveillance is usually recommended. Despite the similar risks, the recommendations are different. First, achalasia is a much rarer condition than BE. While achalasia has an estimated incidence of 1 in 100,000 (40), BE can be present about 10% of GERD patients (41). Second, the EC can appear until 40 years after the initial symptoms of achalasia (1,15,18,19), and third BE has a modifiable precondition. These factors make the evidence more robust with better standardization and more evaluable efficiency.
Another important consideration is that EC has usually a late diagnosis in achalasia since dysphagia caused by the tumor may be attributed to the disease's own symptomatology. Thus, the majority of EC in achalasia is diagnosed in advanced stages, with poor prognosis (19,42,43).
Some factors like age (11,15,19), male gender (10,11,23), time of achalasia (10,11,15,18,19,23), Chagas’ disease (19) are considered risk factors for EC. Other factors such as the type of achalasia treatment (endoscopic versus surgical (18,29,31), alcohol intake and smoking (10), despite plausibility, have less evidence.
Although there is no consensus it seems reasonable to consider endoscopic examination starting from the 10th year of onset of achalasia, every 3 to 5 years, especially in men, elderly, with Chagas' disease, or associated risk factors such as alcohol, smoking and endoscopic treatment for achalasia. However, some questions such as time to start surveillance, the time interval between exams, type of endoscopic technology (white-light, chromoendoscopy or narrow band imaging) and the need for serial biopsies remain unanswered. Further studies are needed for a more robust recommendation.
Conclusions
Achalasia is a recognized risk factor for EC, for both SCC and EAC. The patient must be informed about the risk of EC especially after 10 years, even treated. The treatment of achalasia with methods that increase risk of reflux (botulinum toxin injection, pneumatic dilation and per oral endoscopic myotomy) should be considered as a risk factor for EB.
Surveillance may be considered in patients with more than 10 years of disease, especially if associated with other risk factors.
Acknowledgments
We are indebted to Ms. Cathy Williams, Archives Services Manager from the Archives & Research Collections, King’s College London Archives for her kind attention and authorization to reproduce Figure 1.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the the editorial office, Annals of Esophagus for the series “How Can We Improve Outcomes for Esophageal Cancer?”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoe.2020.02.01). The series “How Can We Improve Outcomes for Esophageal Cancer?” was commissioned by the editorial office without any funding or sponsorship. FAMH served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fagge CH. A case of simple stenosis of the oesophagus, followed by epithelioma. Guys Hosp Rep 1872;17:413-21.
- Rake G. Epithelioma of the oesophagus in association with achalasia of the cardia. Lancet 1931;2:682. [Crossref]
- Kornblum K, Fischer LC. Carcinoma as a complication of achalasia of the cardia. A J R Am J Roentgenol 1940;43:364.
- Ellis FG. Natural History of achalasia of the cardia. Proc R Soc Med 1960;53:663-6. [Crossref] [PubMed]
- Just-Viera JO, Morris JD, Haight C. Achalasia and esophageal carcinoma. Ann Thorac Surg 1967;3:526-38. [PubMed]
- Chino O, Kijima H, Shimada H, et al. Clinicopathological studies of esophageal carcinoma in achalasia: analyses of carcinogenesis using histological and immunohistochemical procedures. Anticancer Res 2000;20:3717-22. [PubMed]
- Pajecki D, Zilberstein B, Cecconello I, et al. Larger amounts of nitrite and nitrate-reducing bacteria in megaesophagus of Chagas’ disease than in controls. J Gastrointest Surg 2007;11:199-203. [Crossref] [PubMed]
- Manoel-Caetano FS, Borim AA, Caetano A, et al. Cytogenetic alterations in chagasic achalasia compared to esophageal carcinoma. Cancer Genet Cytogenet 2004;149:17-22. [Crossref] [PubMed]
- Chuong JJ, DuBovik S, McCallum RW. Achalasia as a risk factor for esophageal carcinoma. A reappraisal. Dig Dis Sci 1984;29:1105-8. [Crossref] [PubMed]
- Leeuwenburgh I, Scholten P, Alderliesten J, et al. Long-term esophageal cancer risk in patients with primary achalasia: a prospective study. Am J Gastroenterol 2010;105:2144-9. [PubMed]
- Sandler RS. The risk of esophageal cancer in patients with achalasia. A population-based study. JAMA 1995;274:1359-62. [Crossref] [PubMed]
- Zaninotto G, Rizzetto C, Zambon P, et al. Long-term outcome and risk of oesophageal cancer after surgery for achalasia. Br J Surg 2008;95:1488-94. [Crossref] [PubMed]
- Rassi A Jr, Rassi A, Marin-Neto JA. Chagas disease. Lancet 2010;375:1388-402. [Crossref] [PubMed]
- Brücher BL, Stein HJ, Bartels H, et al. Achalasia and esophageal cancer: incidence, prevalence, and prognosis. World J Surg 2001;25:745-9. [Crossref] [PubMed]
- Eckardt AJ, Eckardt VF. Editorial: cancer surveillance in achalasia: better late than never? Am J Gastroenterol 2010;105:2150-2. [Crossref] [PubMed]
- Arber N, Grossman A, Lurie B, et al. Epidemiology of achalasia in central Israel. Rarity of esophageal cancer. Dig Dis Sci 1993;38:1920-5. [Crossref] [PubMed]
- Farr CM. Achalasia and esophageal carcinoma: is surveillance justified? Gastrointest Endosc 1990;36:638-9. [Crossref] [PubMed]
- Gillies CL, Farrukh A, Abrams KR, et al. Risk of esophageal cancer in achalasia cardia: A meta-analysis. JGH Open 2019;3:196-200. [Crossref] [PubMed]
- Tustumi F, Bernardo WM, da Rocha JRM, et al. Esophageal achalasia: a risk factor for carcinoma. A systematic review and meta-analysis. Dis Esophagus 2017;30:1-8. [Crossref] [PubMed]
- Globocan. Cancer Incidence, Mortality and Prevalence Worldwide, Version 1.0. lARC Cancer Base No. 5. Lyon: lARC Press, 2000;2001.
- Markar SR, Wiggins T, MacKenzie H, et al. Incidence and risk factors for esophageal cancer following achalasia treatment: National population-based casecontrol study. Dis Esophagus 2019;32:doy106 [Crossref] [PubMed]
- Zaninotto G, Bennett C, Boeckxstaens G, et al. The 2018 ISDE achalasia guidelines. Dis Esophagus 2018;31. [PubMed]
- Zendehdel K, Nyren O, Edberg A, et al. Risk of esophageal adenocarcinoma in achalasia patients, a retrospective cohort study in Sweden. Am J Gastroenterol 2011;106:57-61. [Crossref] [PubMed]
- Guo JP, Gilman PB, Thomas RM, et al. Barrett’s esophagus and achalasia. J Clin Gastroenterol 2002;34:439-43. [Crossref] [PubMed]
- Leeuwenburgh I, Scholten P, Calje TJ, et al. Barrett’s esophagus and esophageal adenocarcinoma are common after treatment for achalasia. Dig Dis Sci 2013;58:244-52. [Crossref] [PubMed]
- Teitelbaum EN, Dunst CM, Reavis KM, et al. Clinical outcomes five years after POEM for treatment of primary esophageal motility disorders. Surg Endosc 2018;32:421. [Crossref] [PubMed]
- Csendes A, Braghetto I, Burdiles P, et al. Very late results of esophagomyotomy for patients with achalasia: clinical, endoscopic, histologic, manometric, and acid reflux studies in 67 patients for a mean follow-up of 190 months. Ann Surg 2006;243:196-203. [Crossref] [PubMed]
- Di Corpo M, Farrell TM, Patti MG. Laparoscopic Heller Myotomy: A Fundoplication Is Necessary to Control Gastroesophageal Reflux. J Laparoendosc Adv Surg Tech A 2019;29:721-5. [Crossref] [PubMed]
- Cantù P, Savojardo D, Baldoli D, et al. Barrett’s esophagus in untreated achalasia: ‘guess who’s coming to dinner’ first. Dis Esophagus 2008;21:473. [Crossref] [PubMed]
- Nesteruk K, Spaander MCW, Leeuwenburgh I, et al. Achalasia and associated esophageal cancer risk: What lessons can we learn from the molecular analysis of Barrett's–associated adenocarcinoma? Biochim Biophys Acta Rev Cancer. 2019;1872: [Crossref] [PubMed]
- Brossard E, Ollyo JB, Fontolliet CH, et al. Achalasia and squamous cell carcinoma of the esophagus: is an endoscopic surveillance justified? Gastroenterology 1992;102.
- Wychulis AR, Woolam GL, Andersen HA, et al. Achalasia and carcinoma of the esophagus. JAMA 1971;215:1638-41. [Crossref] [PubMed]
- Ravi K, Geno DM, Katzka DA. Esophageal cancer screening in achalasia: is there a consensus? Dis Esophagus 2015;28:299-304. [Crossref] [PubMed]
- Hirota WK, Zuckerman MJ, Adler DG, et al. ASGE guideline: the role of endoscopy in the surveillance of premalignant conditions of the upper GI tract. Gastrointest Endosc 2006;63:570-80. [Crossref] [PubMed]
- Vaezi MF, Pandolfino JE, Vela MF. ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol 2013;108:1238-49. [Crossref] [PubMed]
- Ramai D, Lai JK, Ofori E, et al. Evaluation and Management of Premalignant Conditions of the Esophagus: A Systematic Survey of International Guidelines. J Clin Gastroenterol 2019;53:627-34. [Crossref] [PubMed]
- Chaber-Ciopinska A, Kiprian D, Kawecki A, et al. Surveillance of patients at high-risk of squamous cell oesophageal cancer. Best Pract Res Clin Gastroenterol 2016;30:893-900. [Crossref] [PubMed]
- Wani S, Falk G, Hall M, et al. Patients with nondysplastic Barrett’s esophagus have low risks for developing dysplasia or esophageal adenocarcinoma. Clin Gastroenterol Hepatol 2011;9:220-7. [Crossref] [PubMed]
- Wani S, Falk GW, Yerian L, et al. Risk factors for progression of low-grade dysplasia in patients with Barrett’s esophagus. Gastroenterology 2011;141:1179-86. [Crossref] [PubMed]
- Sadowski DC, Ackah F, Jiang B, et al. Achalasia: incidence, prevalence and survival. A population-based study. Neurogastroenterol Motil 2010;22:e256-61. [Crossref] [PubMed]
- Schlottmann F, Patti MG, Shaheen NJ. From Heartburn to Barrett’s Esophagus, and Beyond. World J Surg 2017;41:1698-704. [Crossref] [PubMed]
- Loviscek LF, Cenoz MC, Badaloni AE, et al. Early cancer in achalasia. Dis Esophagus 1998;11:239-47. [Crossref] [PubMed]
- Peracchia A, Segalin A, Bardini R, et al. Esophageal carcinoma and achalasia: prevalence, incidence and results of treatment. Hepatogastroenterology 1991;38:514-6. [PubMed]
Cite this article as: Del Grande LDM, Herbella FAM, Katayama RC, Landini Filho LS, Mocerino J, Ferreira AEP. Achalasia and cancer prevention and surveillance. Ann Esophagus 2020;3:19.


