
Video-assisted thoracoscopic surgery for esophageal duplication cyst recurrence: case report and literature review
Introduction
Esophageal duplication cysts are rare congenital malformations (1), represent approximately 10–15% of all foregut duplication cysts and are typically located in the right postero-inferior mediastinum. Intestinal duplication cysts included enteric duplication cysts, bronchogenic and neuroenteric cysts. It has been observed that at the end of the third week of embryo formation, the dorsal portion of the embryonic intestine elongates to form the esophagus and the ventral portion turn into the respiratory tract. In this phase, errors in the development of the foregut can occurs such as the appearance of bronchogenic cysts and esophageal duplications. Due to this embryological relationship, many experts define these lesions as foregut cysts or foregut duplication errors, without identifying the exact etiology of the mediastinal cysts (2). The diagnosis is histological but, numerous investigations, can help to develop a differential diagnosis. Epidemiological studies report an incidence of one case in 8,200 live births (3), about 70–75% of these cysts are diagnosed in children, the remaining 25–30% are diagnosed in adults. This kind of cyst can be asymptomatic and found incidentally during endoscopy or radiological investigations with Chest-X-Ray, computed tomography (CT) scan or magnetic resonance imaging (MRI) (4,5). The Majority of these cysts are diagnosed in childhood but when present in adults they have more likely symptomatic presentation due to the compression of nearby structures (6). The most common symptoms in these cases are dysphagia, chest pain and respiratory distress such as wheezing and coughing up to aspiration pneumonia. Duplication cysts can be also complicated by intracystic bleeding, perforation and infection, especially those with esophageal communication. Squamous metaplasia may also be present, but instances of malignancy are rare. The diagnosis is histological but, numerous investigations, can help to develop a differential diagnosis. Imaging studies such as chest radiographs and barium swallow studies can reveal a mediastinal mass with esophageal compression along with tracheal displacement and narrowing. Radiological examinations with chest CT scan and/or MRI allow to accurately assess dimensions, the cleavage plan of the mass with neighbouring organs and to differentiate the cystic nature from other possible tumours of the posterior mediastinum (4,7). Esophagus-gastric endoscopy along with endoscopic ultrasound (EUS), helps the differential diagnosis with the solid masses of the mediastinum, identifies the presence of any communications between the lumen of the cyst and the esophageal lumen and allows in selected cases the execution of biopsies and the possibility of endoscopic treatment with puncture and emptying of the cyst through the esophageal wall (5,8). Medical treatment of esophageal duplication cysts is not conclusive and does not improve symptoms; these cysts should be invasive treated even if asymptomatic, as they tend to enlarge over time and can cause serious complications such as obstruction, rupture, bleeding, infection or aspiration resulting in pneumonia (9,10). Invasive treatment consists in surgery with fenestration or complete excision of the cyst; however benign characteristics and the slow evolution push many people to prefer a less invasive approach with endoscopic treatment. We expose the successful case of video-assisted thoracoscopic surgery (VATS) treatment of recurrent esophageal cyst. We present the following article in accordance with the CARE reporting checklist (available at https://aoe.amegroups.com/article/view/10.21037/aoe-2020-26/rc).
Case presentation
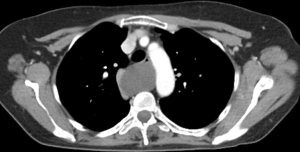
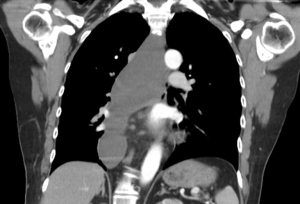
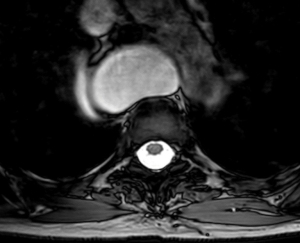
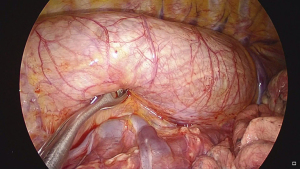
A case of a 59-year-old Caucasian woman, with the appearance in 2002 of progressive dysphagia, first with solids and then with liquids, associated with significant weight loss. The patient underwent EGDS and chest CT scan with contrast, finding an esophageal duplication cysts without communication with the lumen of the esophagus. In September 2003 she underwent surgery to empty and fenestrate the cyst in right triportal VATS with complete regression of symptoms and resumption of normal nutrition. Following the reappearance of dysphagia, the patient was subjected on February 2019 to a new EGDS examination and chest CT scan with contrast which documented recurrence of the cyst as shown in Figure 1, with significantly increased volume compared to the previous one in 2003 (cranio-caudal extension from the root of the neck to the diaphragm for over 24 cm as shown in Figures 2,3, with a diameter of about 7.5×4 cm). Chest MRI with contrast (gadolinium) confirm the cystic nature of the lesion and the presence of clear plane of cleavage with the vertebral column but not with esophageal wall as shown in Figures 4,5. The patient underwent surgery on May 2019 with exeresis of the cyst in right uniportal VATS (intraoperative finding shown in the Figure 6). The duplication cyst was blunt dissected, incised, emptied and excised (as shown in the Video 1). It was not possible to safety remove a small part of cystic wall that was fused with esophageal wall to the upper-third and middle level, site of the previous fenestration. The integrity of the esophageal wall was confirmed by intraoperative EGDS. Histological examination confirmed the esophageal duplication cyst (pathological finding shown in Figure 7). Patient had a regular post-operative course, with pain easily controlled with oral therapy. Feeding with a common diet was early resumed in the first post-operative day with no episodes of dysphagia or regurgitation. Chest tube was removed on the second post-operative day and the patient was discharged. During the follow-up, no chest pain or dysphagia relapse was observed. Control with 6-month chest CT scan showed complete pathological resolution without cystic recurrence. All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.


Discussion
Esophageal duplication cysts represent a rare and benign form of mediastinal tumor. Cyst degeneration in neoplasm has been described by some authors but it’s extremely rare (11,12). Instead, complications of cysts as obstruction, bleeding, infection, or rupture are common and well described (9,10).
Symptomatic patients needed an invasive treatment of the cyst as there are no effective medical therapies. In asymptomatic patients, there are currently no clear guidelines on the treatment to be performed, but most authors agree with the indication for invasive treatment to avoid possible serious complications due to the natural pathological history. Due to the benign nature of this kind of cyst, different invasive treatments have been proposed and used. The review of literature show as many studies reports clinicals outcomes in treatments of inveterate and untreated esophageal duplication cysts. Our intent is to critically evaluate the approach to the treatment of esophageal duplication cysts by paying attention to the problem of recurrence which in many cases makes future minimally invasive approaches difficult if not impossible. The different approaches reported for treatment of this pathology consist in puncture and endoscopic emptying of the cyst, other endoscopic treatments, fenestration or resection of the cyst with thoracoscopic or robotic approach, up to traditional thoracotomy surgery. The most common endoscopic treatments consist of needle aspiration under esophageal ultrasound guide. This technique is often not recommended due to the risk of infection, the high rate of recurrence and the possible appearance of adhesions or leaks with the esophageal wall, which can complicate the pathology and make further surgical resection difficult. Some authors describe endoscopic submucosal tunnel dissection as an option to excise an esophageal bronchogenic cyst (13,14). This kind of cysts are rare, but the technique reported suggests the use of the endoscopic approach to treat esophageal duplication cysts in an effective and minimally invasive way. Other authors reported the results of endoscopic fenestration of esophageal duplication cyst performed by using EUS guidance (15,16). However, there are no studies in the literature showing long-term outcomes and complications after these procedures. For these reasons, many authors suggest that surgery is the best approach to treat esophageal duplication cyst even if asymptomatic (17-19). Surgical treatments consist of fenestration or complete removal of the cyst, usually performed with the thoracotomy technique, however, several cases of cysts removed effectively with minimally invasive technique have been reported in the literature, performed with VATS or robotic-assisted thoracoscopic surgery (RATS). After surgical fenestration or excision, whether it is performed with traditional thoracotomy or with minimally invasive technique, patients’ outcomes are good both in the short term and in the long term. Recurrence is rare but has been reported (20). Complications related to esophageal cyst resection include tracheal and esophageal injuries, pseudodiverticulum development, and nerve injury or paralysis. There are many studies on surgical efficacy in children, however, few studies have investigated indications treatment and postoperative outcomes in adult population. In a case series of twenty-seven patients affected by esophageal duplication cyst and treated by surgical resection, Cioffi et al. showed as minimally invasive surgery guaranteed the same outcomes, a better cosmetic result, less pain, early patient mobilization, lower risk of infectious complications and early discharge (10). In a case series of nine patients, Hazelrigg et al. confirmed similar results (21). Other case reports have shown good postoperative results in patients treated with removal of esophageal duplication cysts with both VATS and RATS techniques (17,19,20,22). Currently, most authors treat recurrences of the cyst with a traditional thoracotomy surgery due to the presence of adhesions, possibility of leak, and local altered anatomy in site of previous treatment, with difficulty or impossibility to recognize a clear limit between esophageal wall and cystic wall. Our case report demonstrates how thoracoscopic treatment can be valid and safe even in cases of recurrences after previous invasive treatments. Benefits of minimally invasive surgery are documented, however there are no studies regarding the thoracoscopic treatment of relapses. Limited number of cases treated and complexity make it difficult to compare thoracotomy and thoracoscopic techniques. The intent of this work is to demonstrate how the minimally invasive approach can be used effectively and safely also in the treatment of recurrences, but future studies with larger numbers of patients will be needed to evaluate the efficacy.
Conclusions
This kind of benign pathology of the thoracic esophagus represents a surgical challenge. Patients, at the same time requiring safe, effective and minimally invasive treatments, have currently shifted attention to techniques performed with an endoscopic approach. In the past, previous chest surgery or failure of minimally invasive approach required traditional thoracotomy surgery. This case shows that minimally invasive surgery, if performed by expert operators, can be used safely even in case of recurrent disease after previous surgery. In the current context, esophageal cystic resection performed with minimally invasive surgery such as VATS technique, represents the suggest therapeutic option for the lower risk of recurrence, best esthetical results, less post-operative pain and the possibility to treat patients underwent previous surgery.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Esophagus for the series “Management of Esophageal Perforations and Injuries and Other Benign Diseases”. The article did not undergo external peer review.
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://aoe.amegroups.com/article/view/10.21037/aoe-2020-26/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoe.amegroups.com/article/view/10.21037/aoe-2020-26/coif). The series “Management of Esophageal Perforations and Injuries and Other Benign Diseases” was commissioned by the editorial office without any funding or sponsorship. VP served as an unpaid Guest Editor of the series. DN served as an unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Esophagus from October 2019 to September 2021. The authors have no other conflicts of interest to declare.
Ethical Statement: All authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Whitaker JA, Deffenbaugh LD, Cooke AR. Esophageal duplication cyst. Case report. Am J Gastroenterol 1980;73:329-32. [PubMed]
- Nobuhara KK, Gorski YC, La Quaglia MP, et al. Bronchogenic cysts and esophageal duplications: common origins and treatment. J Pediatr Surg 1997;32:1408-13. [Crossref] [PubMed]
- Arbona JL, Fazzi JG, Mayoral J. Congenital esophageal cysts: case report and review of literature. Am J Gastroenterol 1984;79:177-82. [PubMed]
- Bondestam S, Salo JA, Salonen OL, et al. Imaging of congenital esophageal cysts in adults. Gastrointest Radiol 1990;15:279-81. [Crossref] [PubMed]
- Liu R, Adler DG. Duplication cysts: Diagnosis, management, and the role of endoscopic ultrasound. Endosc Ultrasound 2014;3:152-60. [Crossref] [PubMed]
- Sonthalia N, Jain SS, Surude RG, et al. Congenital Esophageal Duplication Cyst: A Rare Cause of Dysphagia in an Adult. Gastroenterology Res 2016;9:79-82. [Crossref] [PubMed]
- Rafal RB, Markisz JA. Magnetic resonance imaging of an esophageal duplication cyst. Am J Gastroenterol 1991;86:1809-11. [PubMed]
- Bhatia V, Tajika M, Rastogi A. Upper gastrointestinal submucosal lesions--clinical and endosonographic evaluation and management. Trop Gastroenterol 2010;31:5-29. [PubMed]
- Neo EL, Watson DI, Bessell JR. Acute ruptured esophageal duplication cyst. Dis Esophagus 2004;17:109-11. [Crossref] [PubMed]
- Cioffi U, Bonavina L, De Simone M, et al. Presentation and surgical management of bronchogenic and esophageal duplication cysts in adults. Chest 1998;113:1492-6. [Crossref] [PubMed]
- Lee MY, Jensen E, Kwak S, et al. Metastatic adenocarcinoma arising in a congenital foregut cyst of the esophagus: a case report with review of the literature. Am J Clin Oncol 1998;21:64-6. [Crossref] [PubMed]
- Singh S, Lal P, Sikora SS, et al. Squamous cell carcinoma arising from a congenital duplication cyst of the esophagus in a young adult. Dis Esophagus 2001;14:258-61. [Crossref] [PubMed]
- Tang X, Jiang B, Gong W. Endoscopic submucosal tunnel dissection of a bronchogenic esophageal cyst Endoscopy 2014;46:E626-7. [J]. [Crossref] [PubMed]
- Yang X, Zong Y, Zhao HY, et al. Complete excision of esophageal bronchogenic cyst by endoscopic submucosal tunnel dissection: a case presentation. BMC Gastroenterol 2019;19:155. [Crossref] [PubMed]
- James TW, Grimm IS, Baron TH. Endoscopic fenestration of a symptomatic esophageal duplication cyst. VideoGIE 2017;2:191-2. [Crossref] [PubMed]
- Okamoto T, Nakamura K, Ikeya T, et al. Endoscopic fenestration with EUS guidance for esophageal duplication cyst. VideoGIE 2021;6:211-4. [Crossref] [PubMed]
- Herbella FA, Tedesco P, Muthusamy R, et al. Thoracoscopic resection of esophageal duplication cysts. Dis Esophagus 2006;19:132-4. [Crossref] [PubMed]
- Diehl DL, Cheruvattath R, Facktor MA, et al. Infection after endoscopic ultrasound-guided aspiration of mediastinal cysts. Interact Cardiovasc Thorac Surg 2010;10:338-40. [Crossref] [PubMed]
- Kolomainen D, Hurley PR, Ebbs SR. Esophageal duplication cyst: case report and review of the literature. Dis Esophagus 1998;11:62-5. [Crossref] [PubMed]
- Duan X, Cui Y, He Y, et al. Acute attack of recurrent esophageal duplication cyst in an adult: case report and literature review. J Thorac Dis 2018;10:E335-9. [Crossref] [PubMed]
- Hazelrigg SR, Landreneau RJ, Mack MJ, et al. Thoracoscopic resection of mediastinal cysts. Ann Thorac Surg 1993;56:659-60. [Crossref] [PubMed]
- Obasi PC, Hebra A, Varela JC. Excision of esophageal duplication cysts with robotic-assisted thoracoscopic surgery. JSLS 2011;15:244-7. [Crossref] [PubMed]
Cite this article as: Pogliani L, Zanfrini E, Tabacco D, Meacci E, Margaritora S, Nachira D, Porziella V. Video-assisted thoracoscopic surgery for esophageal duplication cyst recurrence: case report and literature review. Ann Esophagus 2022;5:10.



