
A clinical review of the potential role of microaspiration and a dysregulated aerodigestive microbiome in lung disease
The Human Microbiome Project represents a huge scientific effort to further the understanding of the microbiome and its importance for human life on earth. The initial phase of the project characterized microbial communities in healthy people, with different sites of the body studied (1). This therefore began an ambitious description and understanding of the microbial systems in the body and the role of a normal microbiome, associated with health.
The nasal passages, oral cavity, skin, gastrointestinal (GI) tract, and urogenital tract were studied in the initial phase of the human microbiome project. When initiated, therefore, this massive, frontier scanning, scientific undertaking omitted the lungs and airways from the organ systems studied. This is despite the worldwide importance of lung disease. Chronic obstructive pulmonary disease (COPD), for example, is a disease where clinical exacerbations are often caused by lung infection. With increasing rates, COPD is predicted to become the third leading cause of death by 2030 (2).
The omission of the lungs from the original human microbiome project reflected the textbook understanding that healthy lungs were normally sterile. A reason cited for the historical neglect of the lung in the human microbiome is that sampling the lower airways is considered technically challenging. This is perhaps surprising, as bronchoscopy per se has been a routine procedure for most UK hospitals for the last 40 years. It is arguable that the delayed systematic investigation of the lung microbiome and potential missed insights into lung disease, are related to science being carried out in separate disciplines, with under-connected literature between increasingly specialised research groupings. For example, the sterile lung dogma was maintained despite historical data from careful, elegant radiolabel studies aiming to understand the pathophysiology of pneumonia. Such studies indicated that even in normal people there was overnight oropharyngeal exchange into the lung, consistent with the carriage of a microbiological inoculum. Early molecular characterisation of microbial biofilms in transplanted lungs, in patients without clinical infection, were also described prior to the recent and welcome interest into the lung microbiome.
What is arguably a “rediscovery” of the importance of the human lung microbiome may still underappreciate physiological inter-relationships between organ systems traditionally studied in separate disciplines of translational research. It has been suggested that an important mechanism by which the gut microbiome may affect other organs including the lung is through cross-talk with the gut microbiome. The ‘gut-lung axis’ postulates that gut microbiome metabolites, endotoxins and mediators can be carried into the bloodstream allowing interaction. This therefore may connect the gut and lungs via the circulation, indicating a mechanism by which changes in the diet and gut microbiome may affect lung health (3).
As well as the gut-lung proposal, we have performed work indicating that microaspiration of extra oesophageal refluxate may be an important, direct mechanism through which the lung microbiome is directly modulated. This may be related to an immigration model to understand microbiome ecology and homeostasis (4).
The purpose of this review article, therefore, is to discuss interconnections in the human microbiome, with a focus on aerodigestive pathophysiology and microaspiration (Figure 1). The potential importance of this in human lung disease is discussed and contextualised within the increasing human lung microbiome literature.
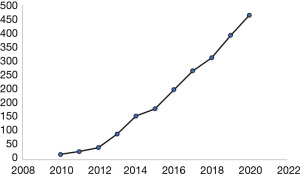
A seminal paper in flagging the importance of the human microbiome was published in 2010 by Hilty et al. (5). The group, led by Professors Moffatt and Cookson, highlighted that the sterile lung paradigm was predicated on data from culture based methods, where healthy airways were seldom studied. It is now better recognised that culture based approaches, while still very important for clinical pathology labs, only detect a minority of bacteria present in complex samples. Microbiology labs if asked would have always observed that different media give different culture results (6), and that single negative cultures are not necessarily a sign of true sterility. Interestingly some of the major microbiological constituents in control subjects, when culture independent molecular techniques were used, were shown to be anaerobes such as Prevotella spp. These organisms can only be grown with advanced culture techniques. The Cookson group pointed out that microbiomes exist even in very hostile environments and that the warm, moist lung environment, would be expected to support a microbiome, from first principles. Their key, sentinel work described changes in the microbiome associated with the asthma airway, priming an explosion of interest in the human lung microbiome in health and disease (Figure 2).
It is of interest that radioisotope studies published by Huxley et al., 30 years prior to the paradigm shifting work of Cookson and colleagues indicated mechanisms which could contribute both to a normal lung microbiome and dysregulation in lung disease (7). In this work small amounts of 111In chloride were placed into the noses of 20 normal subjects, 9 of whom were found to have detectable radiolabel in the lung parenchyma the following day. The authors concluded that sleep was a risk factor for aspiration of upper airway secretions. In further support, 7 of 10 patients with “depressed consciousness” aspirated. Further, quantitative radiolabel measurements were made in 1997 which showed that around 50% of adult normal volunteers had gastric tracer in the lung following sleep, with the quantities of tracer aspirated ranging from 0.01 to 0.2 mL. This order of magnitude was discussed as “likely to contain bacterial organisms in physiologically significant quantities”, an observation made around 13 years before the key work of Cookson and colleagues, outlining a potential lung microbiome (8).
Our group has had a long standing interest in non-alloimmune airway injury in the field of human lung transplantation, dating from the 1990s. This includes the description of “sub clinical” infection. We proposed “that subclinical, persistent infection in the airways is not harmless, but is an added cofactor to airway cellular activation and long-term damage” (9) and a driver of allograft injury related to a finding of elevated levels of soluble CD14 in bronchoalveolar lavage (BAL) fluid from lung allograft recipients. These findings were in the absence of clinical signs of infection including cultured organisms. CD14 is a surface protein, shed following activation, which is found on macrophages and activated neutrophils. It serves as the cellular receptor for lipopolysaccharide, a major component of gram-negative bacteria such as P. aeruginosa and B. cepacia (9).
Many bacteria coordinate gene expression and phenotype in a cell density dependent manner using signal molecules. This quorum sensing has been intensely investigated in P. aeruginosa and B. cepacia lung infection. The formation of antibiotic resistant biofilms is recognised to be controlled by the secretion of chemical quorum signals from bacteria. Our work in lung allograft recipients provided the first evidence that quorum signals were present in the human lung that we are aware of. This was in a series of clinically stable human lung allograft recipients and again showed quorum signals were present in patient BAL samples in the absence of cultured organisms or clinical signs of infection (10). This therefore indicated molecular level evidence of a lung microbiome in lung allograft recipients. While limited to the specialised setting of the lung allograft, our work nevertheless was an early and prescient challenge to the concept of the sterile lung and supportive of subsequent descriptions of a lung microbiome (11).
As well as “sub clinical infection”, our group and others have contributed work showing that gastro-oesophageal reflux and aspiration occurs in lung transplant recipients, representing a potential injury to the vulnerable allograft airways through acid, pepsin and bile acid challenge (12-14). Lung transplant recipients are almost universally treated with proton pump inhibitors (PPI), which reduces gastric acid that is normally microbicidal. We have shown that above pH 4, gastric juice is a source of a culturable microbiome which includes organisms such as P. aeruginosa (15). It is of interest that PPI usage has been associated as a hazard for lung infections including community acquired pneumonia. Recent reports have implicated the use of PPI as a risk factor in the COVID-19 pandemic (16,17). Bacterial numbers present in the upper GI tract, stomach, and small intestine, have been quantified at around 103 to 104 bacteria per mL (18).
The dysregulated lung microbiome present in lung transplant recipients may therefore be directly contributed to by gastroesophageal reflux and aspiration of gastric content. Further evidence to potentially support this hypothesis was provided by the identification of identical strains of P. aeruginosa in the BAL fluid and gastric juice of lung transplant recipients (19). While the swallowing of expectorate into the stomach would be a possible explanation for this finding, another explanation would be aspiration of non-sterile content into the allograft, in recipients consistently shown to have evidence of reflux and aspiration.
Cystic fibrosis (CF) is the most common genetic condition affecting Caucasians and GI problems are a key problem in this multi system disease. Much morbidity and early mortality in CF occurs because of lung disease, and CF is an important indication for lung transplantation. Historically however GI manifestations of CF were responsible for infant death and the importance of the GI system and potential links with lung disease are arguably under-recognised. In a present day assessment of the most important problems, assessed by the broad CF community of patients healthcare professional and carers, GI manifestations of disease were the second ranked of the top ten priorities for UK CF research (20). This includes gastro-oesophageal reflux disease (GORD), which occurs in around 50% of people with CF, who are predominantly treated with PPI (21). We have carried out aerodigestive research to address this priority identified by the CF community. Our studies indicate that the gastric compartment can be a reservoir of microorganisms relevant to CF lung infection and disease progression, with environments that may promote biofilm development. Overall, these findings may be relevant for detection, surveillance and eradication of organisms and suggests potential gut to lung transmission through aspiration, warranting further study (22,23).
Specifically, our work has confirmed a high burden of GI symptoms in people with CF and has identified identical, clonally related strains of Pa were in sputum and gastric juice from the same people with CF (23). The swallowing of expectorated sputa is a normal homeostatic mechanism that could lead to the isolation of identical clonally related microorganisms in the gut and lung environments. Previous studies have also indicated the possibility of microflora exchange between the stomach and the lungs, in children with chronic cough, however (24). We have previously shown markers of non-sterile aspiration in people with CF before and after lung transplantation, indicating the potential translocation of gastric micro-organisms to the lung by microaspiration (13). Our studies have also identified people with CF who had gastric samples with culturable non tuberculosis mycobacteria (NTM) but who had negative sputa, indicating that gastric isolates may be independent from respiratory sources. It is well known in the microbiological literature that NTM can survive in a variety of environments and that gastric sampling for mycobacteria can have a higher diagnostic yield for organisms in clinical studies (23). We therefore propose that cough and other symptoms of extraoesophageal reflux mean that a gastric reservoir could be relevant to transfer of organisms within and between people with CF. Cough aerosols, fomite transmission and aspiration represent potential mechanisms of transfer that could be investigated in future research.
Lung disease in adults with CF is an important cause of bronchiectasis, which is a diagnosis made by medical imaging, demonstrating that the airways of the lungs are abnormally dilated. Bronchiectasis unrelated to a diagnosis of CF is increasingly common in the United Kingdom in an aging population. It has been suggested that the prevalence of bronchiectasis prevalence could be in excess of 300,000 (25).
Hiatal hernia is a recognised risk factor for reflux disease and our group has described an increased prevalence in bronchiectasis with around 35% of patients having radiological evidence, that was related to disease severity (26). The reported prevalence of GORD in bronchiectasis has a wide range from 11–75%, which indicates the importance of objective measurement of reflux for this and other chronic lung diseases. Large studies have prospectively indicated an association between GORD symptoms, increased exacerbations and hospitalisations and reduced quality of life (27,28). Increased bacterial colonisation and a decrease in lung function also indicate a potential role for reflux and microaspiration. It is of interest that small studies have shown the presence of pepsin in sputum (29) and exhaled breath (30) in people with bronchiectasis indicating potential microaspiration. The potential importance of this and the need for better understanding of aerodigestive pathophysiology in bronchiectasis is emphasised by the finding of increased mortality associated with GORD in both a single centre and multi-centre study of bronchiectasis patients (31,32). Multi-disciplinary studies investigating aerodigestive pathophysiology in bronchiectasis and other chronic lung diseases are currently underway (33).
In addition to chronic airway suppurative pathophysiology such as CF and bronchiectasis, reflux and aspiration have consistently been implicated in the pathophysiology of diseases traditionally recognised as parenchymal. Idiopathic pulmonary fibrosis (IPF) is a rare disease, but is increasing in prevalence. With a median mortality of 50% 3 years after diagnosis this is a very serious health problem. Therapeutic options, which include lung transplantation are limited. In a mixed disciplinary aerodigestive evaluation of people with IPF we showed a high burden of symptoms and objective evidence of reflux in 22 of 36 patients studied (61%). Appoximately 50% of our patients had abnormal levels of reflux at ambulatory pH impedance monitoring. Patients with reflux were found to have elevated levels of pepsin in BAL, indicating that gastric aspiration may occur and the potential utility of markers of aspiration in aerodigestive studies (34). In another study hiatal hernias were shown to be significantly more prevalent in IPF (39%) than COPD (13.3%, P=0.00009) or asthma (16.67%, P=0.0139) patients. In IPF, however, hiatal hernia did not correlate with worse lung function (35).
Treatment for GORD is common in people with IPF, despite limited trial data. This has ranged from medical management through to consideration of anti-reflux surgery in some centres. There has been a high profile, multi-centre phase 2 trial evaluation of surgical fundoplication in people with IPF, reflecting the interest regarding the role of GORD in contributing to IPF lung disease (36). Our aerodigestive studies in IPF would indicate the need for a cautious approach to fundoplication in IPF. We showed high levels of oesophageal dysfunction at manometry. This may have been age related but links between dysmotility and IPF have been demonstrated by others (37), as well as ourselves. This is important because oesophageal dysmotility can affect normal swallowing after fundoplication and detection is regarded as mandatory in many centres. After formal MDT review, our experience was that fundoplication was only recommended for a minority of IPF patients a group of patients who usually are frail and elderly and who have many comorbidities.
Apart from surgical intervention, treatment with PPIs is very common in IPF despite a lack of published evidence for this. In a very rare, pilot randomised controlled trial of Omeprazole in IPF, a small excess of lower respiratory tract infections were shown (38). A larger multi-centre trial of PPI therapy in IPF is now underway in the UK, which will provide further information on the role of PPI therapy in this patient group (39).
As well as reflux and microaspiration a dysregulated lung microbiome has recently been implicated in the pathophysiology of IPF, and acute exacerbations of disease. It is of interest that recent study has indicated a role for the presence of lung firmicutes in the pathophysiology of IPF and other interstitial lung diseases, and confirmed the finding that a high bacterial load at diagnosis predicted the subsequent progression of IPF (40).
We suggest that further aerodigestive research is required to study for bacterial translocation during reflux and aspiration in people with IPF. Aspiration of a range of organisms could cause injury. As well as the general dysregulated microbiome documented in the lungs of people with IPF (36), investigation of specific candidate organisms may be of interest. The highly prevalent gram-ve organism H. pylori could cause direct injury to airway epithelia for example. Investigating possible indirect injury through aspiration of vacuolating cytotoxin (VacA) and the cytotoxin-associated gene (CagA), associated with H. pylori, may also produce insights into this and other lung disease (41).
As well as aspiration related to reflux the authors feel that the importance of dysphagia in chronic lung disease, will be increasingly recognised as a source of ageing and frailty related microbiome exchange between the oropharynx and the lung (Figure 1). This is inter-related with but different from aspiration linked to reflux. This may offer much needed, new approaches for multi-disciplinary treatment, such as speech and language therapy. Our preliminary experience indicates dysphagia related microaspiration may have a role in non-CF Bronchiectasis (42). In IPF, we showed in a pilot study of 10 unselected patients that three had airway penetration on videofluoroscopy imaging and that one patient aspirated liquid without a cough response (43). Dysphagia is likely to be an important and arguably neglected element of pathophysiology in other chronic lung diseases including COPD. We therefore conclude that an increased broad understanding of microaspiration, and potential aetiologies, is an important area of research. This may be relevant to a broad range of lung pathophysiologies and new pathways of treatment.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Esophagus for the series “Epidemiology, Biomarkers and Modelling of Gastroesophageal Reflux Disease”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://aoe.amegroups.com/article/view/10.21037/aoe-20-88/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoe.amegroups.com/article/view/10.21037/aoe-20-88/coif). The series “Epidemiology, Biomarkers and Modelling of Gastroesophageal Reflux Disease” was commissioned by the editorial office without any funding or sponsorship. JP served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- NIH Human Microbiome Project. c2020. Available online: https://www.hmpdacc.org/hmp/
- Chronic respiratory diseases: COPD predicted to be third leading cause of death in 2030. 20 May 2008. Available online: https://www.who.int/respiratory/copd/World_Health_Statistics_2008/en/
- Raftery AL, Tsantikos E, Harris NL, et al. Links between inflammatory bowel disease and chronic obstructive pulmonary disease. Front Immunol 2020;11:2144. [Crossref] [PubMed]
- Dickson RP, Erb-Downward JR, Martinez FJ, et al. The microbiome and the respiratory tract. Annu Rev Physiol 2016;78:481-504. [Crossref] [PubMed]
- Hilty M, Burke C, Pedro H, et al. Disordered microbial communities in asthmatic airways. PLoS One 2010;5:e8578. [Crossref] [PubMed]
- Stephenson D, Perry A, Appleby MR, et al. An evaluation of methods for the isolation of nontuberculous mycobacteria from patients with cystic fibrosis, bronchiectasis and patients assessed for lung transplantation. BMC Pulm Med 2019;19:19. [Crossref] [PubMed]
- Huxley EJ, Viroslav J, Gray WR, et al. Pharyngeal aspiration in normal adults and patients with depressed consciousness. Am J Med 1978;64:564-8. [Crossref] [PubMed]
- Gleeson K, Maxwell SL, Eggli DF. Quantitative aspiration during sleep in normal subjects. Chest 1997;111:1266-72. [Crossref] [PubMed]
- Ward C, Walters EH, Zheng L, et al. Increased soluble CD14 in bronchoalveolar lavage fluid of stable lung transplant recipients. Eur Respir J 2002;19:472-8. [Crossref] [PubMed]
- Ward C, Cámara M, Forrest I, et al. Preliminary findings of quorum signal molecules in clinically stable lung allograft recipients. Thorax 2003;58:444-6. [Crossref] [PubMed]
- Moffatt MF, Cookson WO. The lung microbiome in health and disease. Clin Med (Lond) 2017;17:525-9. [Crossref] [PubMed]
- Aldhahrani A, Verdon B, Ward C, et al. Effects of bile acids on human airway epithelial cells: implications for aerodigestive diseases. ERJ Open Res 2017;3:00107-2016. [Crossref] [PubMed]
- Brodlie M, Aseeri A, Lordan JL, et al. Bile acid aspiration in people with cystic fibrosis before and after lung transplantation. Eur Respir J 2015;46:1820-3. [Crossref] [PubMed]
- Griffin SM, Robertson AG, Bredenoord AJ, et al. Aspiration and allograft injury secondary to gastroesophageal reflux occur in the immediate post-lung transplantation period (prospective clinical trial). Ann Surg 2013;258:705-11; discussion 711-2. [Crossref] [PubMed]
- Jones R, Pearson J, Ward C. Functional dyspepsia. N Engl J Med 2016;374:895. [Crossref] [PubMed]
- Almario CV, Chey WD, Spiegel BMR. Increased risk of COVID-19 among users of proton pump inhibitors. Am J Gastroenterol 2020;115:1707-15. [Crossref] [PubMed]
- Lee SW, Ha EK, Yeniova AÖ, et al. Severe clinical outcomes of COVID-19 associated with proton pump inhibitors: a nationwide cohort study with propensity score matching. Gut 2021;70:76-84. [Crossref] [PubMed]
- Hillman ET, Lu H, Yao T, et al. Microbial ecology along the gastrointestinal tract. Microbes Environ 2017;32:300-13. [Crossref] [PubMed]
- Krishnan A, Perry A, Robertson A, et al. Identical biofilm forming strains of pseudomonas aeruginosa occur in lung allograft BAL and gastric juice from cf patients with gastro oesophageal reflux. J Heart Lung Transplant 2013;32:S28.
- Rowbotham NJ, Smith S, Leighton PA, et al. The top 10 research priorities in cystic fibrosis developed by a partnership between people with CF and healthcare providers. Thorax 2018;73:388-90. [Crossref] [PubMed]
- Blondeau K, Dupont LJ, Mertens V, et al. Gastro-oesophageal reflux and aspiration of gastric contents in adult patients with cystic fibrosis. Gut 2008;57:1049-55. [Crossref] [PubMed]
- Al-Momani H, Perry A, Stewart CJ, et al. Microbiological profiles of sputum and gastric juice aspirates in Cystic Fibrosis patients. Sci Rep 2016;6:26985. [Crossref] [PubMed]
- Al-Momani H, Perry A, Jones R, et al. Nontuberculous mycobacteria in gastrostomy fed patients with cystic fibrosis. Sci Rep 2017;7:46546. [Crossref] [PubMed]
- Rosen R, Hu L, Amirault J, et al. 16S community profiling identifies proton pump inhibitor related differences in gastric, lung, and oropharyngeal microflora. J Pediatr 2015;166:917-23. [Crossref] [PubMed]
- Bronchiectasis statistics. c2020. Available online: https://statistics.blf.org.uk/bronchiectasis
- McDonnell MJ, Ahmed M, Das J, et al. Hiatal hernias are correlated with increased severity of non-cystic fibrosis bronchiectasis. Respirology 2015;20:749-57. [Crossref] [PubMed]
- McDonnell MJ, Das J, O’Toole D, et al. Effects of gastro-oesophageal reflux and duodeno-gastro-oeophageal microaspiration in bronchiectasis. Eur Respir J 2018;52:4950.
- McDonnell M, Rutherford R, De Soyza A, et al. The association between gastro-oesophageal reflux and exacerbations of bronchiectasis: data from the EMBARC registry. Eur Respir J 2017;50:abstr OA1968.
- Lee AL, Button BM, Denehy L, et al. Proximal and distal gastro-oesophageal reflux in chronic obstructive pulmonary disease and bronchiectasis. Respirology. 2014;19:211-7. [Crossref] [PubMed]
- Lee AL, Button BM, Denehy L, et al. Exhaled breath condensate pepsin: potential noninvasive test for gastroesophageal reflux in COPD and bronchiectasis. Respir Care 2015;60:244-50. [Crossref] [PubMed]
- McDonnell MJ, Aliberti S, Goeminne PC, et al. Comorbidities and the risk of mortality in patients with bronchiectasis: an international multicentre cohort study. Lancet Respir Med 2016;4:969-79. [Crossref] [PubMed]
- McDonnell MJ, O'Mahony M, Breen D, et al. Increased disease severity and mortality associated with the bronchiectasis-GORD phenotype. Eur Respir J 2015;46:abstr PA366.
- McDonnell MJ, Hunt EB, Ward C, et al. Current therapies for gastro-oesophageal reflux in the setting of chronic lung disease: state of the art review. Eur Respir J Open Res 2020;6:00190-2019. [Crossref] [PubMed]
- Jones R, Krishnan A, Zeybel GL, et al. Reflux in idiopathic pulmonary fibrosis: treatment informed by an integrated approach. ERJ Open Res 2018;4:00051-2018. [Crossref] [PubMed]
- Noth I, Zangan SM, Soares RV, et al. Prevalence of hiatal hernia by blinded multidetector CT in patients with idiopathic pulmonary fibrosis. Eur Respir J 2012;39:344-51. [Crossref] [PubMed]
- Raghu G, Pellegrini CA, Yow E, et al. Laparoscopic anti-reflux surgery for the treatment of idiopathic pulmonary fibrosis (WRAP-IPF): a multicentre, randomised, controlled phase 2 trial. Lancet Respir Med 2018;6:707-14. [Crossref] [PubMed]
- D'Ovidio F, Singer LG, Hadjiliadis D, et al. Prevalence of gastroesophageal reflux in end-stage lung disease candidates for lung transplant. Ann Thorac Surg 2005;80:1254-60. [Crossref] [PubMed]
- Dutta P, Funston W, Mossop H, et al. Randomised, double-blind, placebo-controlled pilot trial of omeprazole in idiopathic pulmonary fibrosis. Thorax 2019;74:346-53. [Crossref] [PubMed]
- Treating people with idiopathic pulmonary fibrosis with the addition of lansoprazole (TIPAL). Last edited 15/
10/2020. Available online: http://www.isrctn.com/ISRCTN13526307 - Invernizzi R, Wu BG, Barnett J, et al. The respiratory microbiome in chronic hypersensitivity pneumonitis is distinct from that of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2021;203:339-47. [Crossref] [PubMed]
- Kanbay M, Kanbay A, Boyacioglu S. Helicobacter pylori infection as a possible risk factor for respiratory system disease: a review of the literature. Respir Med 2007;101:203-9. [Crossref] [PubMed]
- Brennan M, McDonnell MJ, Ward C, et al. Bronchiectasis in the elderly—a disease that has not gone away Michelle Brennan. Current Geriatrics Reports 2020;9:19-29.
- Alamer A, Jones R, Ward C, et al. Oropharyngeal swallowing pathophysiology in patients with idiopathic pulmonary fibrosis: a consecutive descriptive case series. Eur Respir J 2020;56:3370. [Crossref] [PubMed]
Cite this article as: Althuwaybi A, Alamer A, McDonnell MJ, Brennan M, Rutherford RM, Wilcox M, Chater P, Pearson J, Ward C. A clinical review of the potential role of microaspiration and a dysregulated aerodigestive microbiome in lung disease. Ann Esophagus 2023;6:7.



