Treatment of a benign esophagopericardial fistula with an esophageal stent—a case report
Introduction
Esophagopericardial fistulas are associated with both benign and malignant disease. Patients often present with chest pain and shortness of breath and are sometimes in extremis. Treatment involves pericardial drainage with pericardiocentesis or pericardial window, followed by source control with esophageal stent or diversion. Mortality rates are high due to the severity of the disease as well as the association with aggressive malignancy. We present a case of a patient who developed a benign esophagopericardial fistula, despite a history of gastric adenocarcinoma treated with gastrectomy. She was treated with a pericardial window and esophageal stent and was doing well 1.5 years after treatment. Unlike previously described cases of esophagopericardial fistula in which patients underwent stent removal within 2 months of placement or did not have follow-up, our patient was quite frail and did not want any further interventions after stent placement. We present the case in accordance with the CAse REport (CARE) Guidelines.
Case presentation
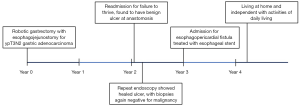
A 74-year-old woman with a history of gastric cancer presented to her local emergency department with severe chest pain (Figure 1). About 3 years earlier, she received neoadjuvant chemotherapy and underwent robotic partial gastrectomy for ypT3N2 gastric adenocarcinoma. About 1 year after completion of treatment, she was admitted for failure to thrive, and upper endoscopy showed an ulcer at the esophagogastric anastomosis. Biopsies of the ulcer were negative for malignancy, and she was treated medically. Repeat endoscopy a few months later showed that the ulcer had healed, and biopsies of the esophagus were again negative for malignancy.
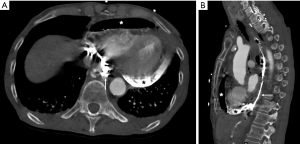
On arrival to the hospital, she was found to be tachycardic, hypotensive, and cachectic. Computed tomography (CT) scan of the chest with oral contrast showed contrast and air in the pericardial space, suggesting a large esophagopericardial fistula (Figure 2). She was transferred urgently to our institution. Urgent subxiphoid pericardial window was performed, but there was only a small amount of serous fluid. Upper endoscopy showed a 2-cm opening in the anterior wall of the esophagus at the esophagogastric anastomosis at 35 cm from the incisors. The beating heart covered in fibrinous material could be seen thru the opening (Video 1). The surrounding esophageal mucosa appeared normal. An esophageal stent (EndoMaxx, Merit Medical, South Jordan, UT, USA) with diameter 23 mm and length 15 cm was placed with endoscopic and fluoroscopic guidance.
Cytologic examination of the pericardial fluid showed abundant acute inflammation and scattered squamous cells, but no evidence of malignancy. Pathologic examination of the pericardium showed dense acute and chronic inflammation, with granulation tissue and adherent fibrin, consistent with pericarditis. The esophageal biopsy showed squamocolumnar mucosa with necrotic exudate and no evidence of malignancy.
Postoperatively, the patient had delirium that resolved over several days. She had a few episodes of rapid atrial fibrillation that resolved with metoprolol. She underwent percutaneous endoscopic jejunostomy tube placement and was started on tube feeding. She improved clinically but was very deconditioned and decided she did not want any further interventions. She was discharged to a nursing facility with hospice care, with the esophageal stent in place, on tube feeds and sips for comfort.
She was seen in clinic at 6 weeks and reported persistent chest pain. She was still deconditioned and unable to stand. At 1.5 years after the procedure, she was living at home and independent in her activities of daily living. Hospice care had been discontinued. She was eating a regular diet but still relied on tube feeds.
Discussion
Esophagopericardial fistulas are associated with benign and malignant disease. Malignant esophagopericardial fistulas often develop as patients are treated for known esophageal cancer (1,2), but can also be the presenting pathology that leads to the diagnosis of malignancy (3-5). Benign esophagopericardial fistulas are most commonly due to ulcer disease (6) and foreign body such as esophageal stent (7), endoscopic drains (8), or fish bone (9,10). They have also been reported after cardiac ablation for atrial fibrillation (11-13) and infection (14). This case highlights the possibility of a benign etiology even when the patient has a history of malignant disease.
Treatment of esophagopericardial fistula traditionally involved surgical diversion with esophagectomy and cervical esophagostomy (15,16), but more recently has involved more esophageal stent placement (1,2,7). Esophageal stents were approved for use in 1845 and have been associated with both development (7) and treatment (1,2,13) of esophagopericardial fistulas. In previously described cases, esophageal stents were removed within 2 months of placement (11,17,18) or the patient died (1) or did not have follow-up (2). In contrast, our patient survived to 1.5 years after stent placement, and she chose not to have endoscopic surveillance or further treatment.
Unfortunately, the mortality rate for patients with malignant esophagopericardial fistula is extremely high, due to the nature of this pathology as well as advanced underlying disease. Successful treatment with single-stage esophagectomy and reconstruction has been reported in a patient who had just completed neoadjuvant chemotherapy for distal esophageal squamous cell carcinoma (19). In that case, pericardial fluid cytology was negative for malignancy, and surgical pathology showed a complete pathologic response.
This patient had a benign esophagopericardial fistula despite a history of gastric adenocarcinoma treated by gastrectomy. She developed a persistent benign ulcer at her esophagojejunal anastomosis that perforated into her pericardial space. She was quite frail and not a surgical candidate. After palliative esophageal stent placement, she did not want further treatment and was discharged to a skilled nursing facility with hospice. Fortunately, she recovered smoothly and was enjoying life 1.5 years later with the stent still in place. Strengths of this case report include a unique etiology of the esophagopericardial fistula due to benign ulcer disease, despite a history of malignancy, as well as the clear demonstration of the fistula on CT images and endoscopic video. Limitations of this case report include the lack of very long-term follow-up or active surveillance for risks of chronic stent placement such as migration or recurrent fistula. While we do not recommend routine placement of long-term esophageal stents, this patient felt that she benefited from this less invasive procedure. This case highlights that esophageal stent placement should be considered in patients with esophagopericardial fistulas, especially when the etiology is benign, and in patients who are poor surgical candidates.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoe.2020.03.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nakshabendi IM, Havaldar S, Nord HJ. Pyopneumopericardium due to an esophagopericardial fistula: treatment with a coated expandable metal stent. Gastrointest Endosc 2000;52:689-91. [Crossref] [PubMed]
- Tukkie R, Hulst RWM, Sprangers F, et al. Tukkie - An esophagopericardial fistula successfully treated with an expandable covered metal mesh stent. Gastrointest Endosc 1996;43:165-7. [Crossref] [PubMed]
- Kohl O, Schaffer R, Doppl W. Purulent pericarditis as an initial manifestation of esophageal carcinoma. Dtsch Med Wochenschr 1999;124:381-5. [Crossref] [PubMed]
- Tombazzi C, Marino G, Yong J, et al. Malignant esophageal pericardial fistula presenting as cardiac tamponade. Dig Dis Sci 2006;51:1290-3. [Crossref] [PubMed]
- Włodarczyk J, Olechnowicz H, Kocon P. Esophago-pericardial fistula during the course of primary esophageal carcinoma. Ann Thorac Surg 2008;86:1967-9. [Crossref] [PubMed]
- Miller WL, Osborn MJ, Sinak LJ, et al. Pyopneumopericardium Attributed to an Esophagopericardial Fistula: Report of a Survivor and Review of the Literature. Mayo Clinic Proceedings 1991;66:1041-5. [Crossref] [PubMed]
- Farkas ZC, Pal S, Jolly GP, et al. Esophagopericardial Fistula and Pneumopericardium From Caustic Ingestion and Esophageal Stent. Ann Thorac Surg 2019;107:e207-8. [Crossref] [PubMed]
- Meunier H, Menahem B, Mulliri A, et al. Esophagopericardial fistula: an unexpected dreaded complication of treatment of leak following revisional sleeve gastrectomy by endoscopic internal drainage. J Surg Case Rep 2017;2017:rjx049 [Crossref] [PubMed]
- Choi JB, Lee SY, Jeong JW. Delayed diagnosis of purulent pericarditis caused by esophagopericardial fistula by computed tomography scan and echocardiography. Eur J Cardiothorac Surg 2001;20:1267-9. [Crossref] [PubMed]
- Kim TH, Kim SW, Seo GS, et al. Pyopneumopericardium due to an esophagopericardial fistula with a fish bone. Am J Gastroenterol 2003;98:1441-2. [Crossref] [PubMed]
- Eitel C, Rolf S, Zachaus M, et al. Successful nonsurgical treatment of esophagopericardial fistulas after atrial fibrillation catheter ablation: a case series. Circ Arrhythm Electrophysiol 2013;6:675-81. [Crossref] [PubMed]
- Giacomino BD, Worden N, Marchigiani R, et al. Pericardial-esophageal fistula complicating cryoballoon ablation for refractory atrial fibrillation. HeartRhythm Case Rep 2017;3:2-6. [Crossref] [PubMed]
- Quénéhervé L, Musquer N, Leaute F, et al. Endoscopic management of an esophagopericardial fistula after radiofrequency ablation for atrial fibrillation. World J Gastroenterol 2013;19:3352-3. [Crossref] [PubMed]
- Al-Ajmi J, Al-Soub H, El-Deeb Y. Pyopneumopericardium due to esophago-pericardial fistula in patient with tuberculous pericarditis. Saudi Med J 2007;28:969-70. [PubMed]
- Shah S, Saum K, Greenwald BD, et al. Esophagopericardial fistula arising from Barrett's esophagus. Am J Gastroenterol 1998;93:465-7. [Crossref] [PubMed]
- Welch TG, White TR, Lewis RP, et al. Esophagopericardial fistula presenting as cardiac tamponade. Chest 1972;62:728-31. [Crossref] [PubMed]
- Dy RM, Harmston GE, Brand RE. Treatment of malignant esophagopericardial fistula with expandable metallic stents in the presence of esophageal varices. Am J Gastroenterol 2000;95:3292-4. [Crossref] [PubMed]
- Gubler C, Bauerfeind P. Successful closure of an esophagopericardial fistula with an over-the-scope clip. Endoscopy 2012;44 Suppl 2 UCTN:E194-5.
- Vardas PN, Acton MD, Rosati CM, et al. One-stage surgical management of an esophagopericardial fistula presenting with tamponade. J Thorac Cardiovasc Surg 2019;158:e143-5. [Crossref] [PubMed]
Cite this article as: Wang Y, Liou DZ, Tsai EB, Lui NS. Treatment of a benign esophagopericardial fistula with an esophageal stent—a case report. Ann Esophagus 2020;3:30.