Per-oral endoscopic myotomy (POEM): overview and experience of 100 cases by a single surgeon in Australia
Introduction
Achalasia is a rare motility disorder of the oesophagus traditionally reported as affecting up to 1.6 to 2.8 per 100,000 individuals (1,2). It is associated with impaired oesophageal motility which may be partial or absent and is also associated with incomplete or absent relaxation of the lower oesophageal sphincter (LOS). In association with swallowing, this effectively results in a functional obstruction of the oesophagus. Treatment is directed at overcoming this obstruction, principally by reducing pressures at a LOS. The current treatment modalities include oesophageal balloon dilatation, laparoscopic Heller myotomy (LHM) and most recently per-oral endoscopic myotomy (POEM). By reduction in the pressure of the LOS, these treatments aim to improve symptomatic dysphagia without addressing the underlying cause.
What are the origins of POEM?
Endoscopic myotomy in the treatment of achalasia was first introduced by Ortega et al. in 1980 with a case series of 17 patients (3). Incisions were made at the distal end of the oesophageal rosette. Results were encouraging, with a significant reduction in oesophageal pressure. During the period of follow-up between 3 and 25 months, patients experienced an improvement in their dysphagia and average weight gains of 5 kg. There were no critical adverse events.
Despite success in this small cohort of patients, further investigation into an endoscopic myotomy for achalasia was not published until 2007 in a porcine model by Pasricha et al. (4).
The technique was modified to create a submucosal working channel through a nick in the oesophageal mucosa 5 cm above the gastro-oesophageal junction. A submucosal saline lift was used and a controlled radial expansion balloon was also used to create the tunnel. The circular layer of muscle was incised, and clips were applied to close the mucosal defect. Pre- and post-operative manometry revealed a significant reduction in LOS pressures from 16.4 to 6.7 mmHg.
Subsequently, POEM has evolved out of the Natural Orifice Transluminal Endoscopic Surgery (NOTES) era and it has been the most lasting development from this time. POEM was described by Inoue et al. in 2010 (5). The first procedure was performed in September 2008 on 17 consecutive patients with achalasia, including patients with either sigmoid or non-sigmoid oesophagus. Oesophageal manometry was undertaken pre- and post-procedure. POEM was described as successful in all cases.
This was followed up with a much larger study published in 2020, involving 1,346 patients who underwent POEM (6). Patients were evaluated pre-operatively with Eckardt scores, oesophageal manometry, endoscopy, barium swallow and computerised tomography (CT). The procedure was performed in 8 centres, by surgeons who had learned the POEM procedure from Professor Inoue. Patient outcomes were deemed successful if the Eckardt score was less than or equal to 3. Treatment success was shown in 95.1% of patients at 6 months and 94.7% of patients at 1 year. The mean length of oesophageal myotomy was 10.8 cm with a mean length of gastric myotomy of 2.8 cm. There was a 3.7% complication rate with 0.4% of patients experiencing mucosal perforation. There were no patients with a complication of Clavien-Dindo classification grade IIIb or above.
On this basis POEM has become widely practiced across the world, frequently as the primary treatment for oesophageal achalasia.
What are the indications and contraindications for POEM and which patients are suitable?
POEM provides a new access portal for the division of the LOS and whilst it is in principle the same operation as a LHM, the access provides a unique advantage. Not only can POEM be used as a first line treatment for achalasia, but it is valuable in several clinical settings where transabdominal access is difficult or not possible. These situations include:
- Revisional procedures after a previous LHM;
- In the setting of a hostile abdominal environment—such as previous upper abdominal surgery especially if this has been associated with complications;
- Abdominal adhesions from any cause.
In addition to these indications POEM can be performed after a previous failed POEM. The advantages in many of these settings is that access is not via scarred tissues which would increase the risk of perforation and also that the myotomy can be performed in an area of the oesophagus that has not previously had surgery for example posteriorly after an anterior myotomy. In this setting a POEM has a clear advantage over LHM.
Although most patients are suitable for POEM, several contraindications or relative contraindications have been suggested including (7):
- Patients unfit for a general anaesthetic;
- Previous oesophageal rupture;
- Severe oesophagitis;
- Coagulation disorders;
- Prior radiation causing submucosal fibrosis;
- Large hiatal hernias or diverticulum;
- Barrett’s oesophagus;
- Young patients.
Most of the contraindications are relative, however an absolute contraindication is when a patient is unfit for a general anaesthetic. A previous rupture may present difficulties accessing the submucosal plane and a large hiatus hernia may also present anatomical difficulties. General factors such as coagulopathy may also be a relative contraindication, as this can generally be corrected. Obesity may also present difficulties increasingly as the population incidence of obesity increases. Patients with Barrett’s oesophagus may have a higher cancer risk due to reflux post-POEM. Similarly, young patients who might end up with a lifetime of reflux may develop Barrett’s Oesophagus. In one study, asymptomatic Barrett’s oesophagus was identified in 7% of patients 5 years post-cardiomyotomy (8).
Methods
Patient investigation and preparation
A clinical history and examination are undertaken and once a diagnosis is made the Eckardt score is determined (9).
Oesophageal manometry is performed to confirm the diagnosis of achalasia and classify the type of achalasia according to the Chicago Classification (10). In some circumstances, contrast imaging may be obtained with a barium swallow or CT which can provide anatomical information. Other general investigations are performed as appropriate as part of the preoperative workup.
Prior to surgery all patients are investigated with gastroscopy to exclude secondary causes such as a small tumour at the oesophagogastric junction resulting in secondary achalasia. This also provides a guide to the amount of oesophageal content and degree of dilatation. If there is a large amount of oesophageal food content, patients are placed on a fluid diet for several days prior to the POEM procedure. This reduces the amount of oesophageal washout that needs to be done on the day of the procedure.
Equipment
The POEM technique used by the author is similar to that described elsewhere (5). Equipment includes a standard high definition gastroscope with a short dissecting cap, a triangular tipped knife, an ERBE diathermy machine, an endoscopic injecting needle as well as endoscopic diathermy forceps. Clips are used for mucosotomy closure. The submucosal dissecting fluid used is saline with methylene blue and CO2 is used for insufflation of the submucosal space.
Procedure
Patients are admitted on the day of surgery and the procedure is undertaken with the patient in a supine position under general anaesthetic. A single dose of antibiotics is given. The abdomen is prepped in case intraabdominal gas needs to be decompressed with a Verres needle.
A gastroscopy is performed to ensure that the lumen of the oesophagus is clear and if necessary, irrigation is undertaken with aqueous chlorhexidine.
Four measurements are documented:
- The site of the mucosotomy;
- The start of the myotomy which is commenced at least 2 cm below the mucosotomy;
- The esophago-gastric junction (EGJ) and
- The lowest point of the myotomy which is the stomach wall 2 cm below the EGJ.
It is essential that the myotomy is adequately extended on to the gastric side of the EGJ to reduce the long-term symptomatic recurrence rates (11).
The length of the myotomy is determined on an individual patient basis. Patients with type III achalasia on average have a longer myotomy with the aim of overcoming the pain associated with spasm.
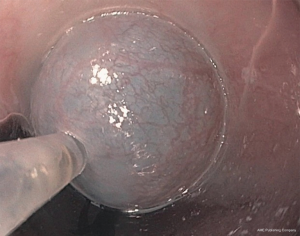
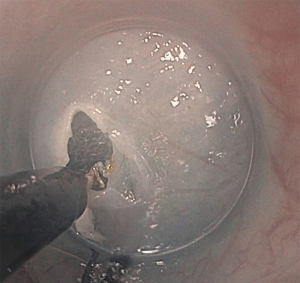
The procedure commences with a submucosal lift injection of 10ml saline with methylene blue (Figure 1). The submucosal space is then opened to allow the gastroscope with dissecting cap to enter the submucosal plane. The 1.5-cm mucosotomy is most commonly oriented longitudinally which allows for easier closure but can be done transversely. This plane is opened by insufflating with CO2 (Figure 2).
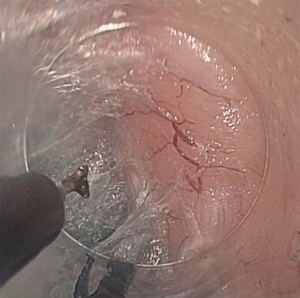
A submucosal tunnel (Figure 3) is then created by dividing the submucosal tissue with a combination fluid injection and diathermy. It is important that the submucosal tunnel continues on to the gastric side of the EGJ. Dissection is kept close to the circular muscle layer to avoid mucosal injury.
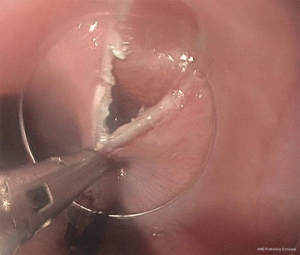
The triangular tipped diathermy knife is then used to divide the inner circular layer of oesophageal muscle in an antegrade fashion (Figure 4) from 2 cm below the mucosotomy down on to the proximal gastric wall. The relaxation of the LOS is confirmed by passing the gastroscope through the native lumen of the oesophagus. The mucosal entry point is closed with a series of clips (Figure 5).
Occasionally the abdomen becomes distended with CO2 and decompression may be required. This can be safely done with a Verres needle. Subcutaneous emphysema is also not uncommon in the tissues of the head and neck.
Post procedure care
Post-operatively patients commence fluids and progress to soft food within 24 hours. A contrast swallow was performed early in our experience however this has been abandoned unless there is a concern about a mucosal breach. Patients are discharged within 24 to 48 hours.
Results
The first POEM procedure in Australia was undertaken was in 2013 by the main author and this paper reports the experience of the first one hundred POEM procedures. These were done between October 2013 and November 2019.
The data was collected prospectively. All patients underwent preoperative manometry and the majority had an endoscopy performed by the surgeon prior to the POEM. Subsequent to the procedure the patients were seen at 3 weeks, 3 months and 1 year. Gastroscopy was performed at 3 months to assess for the presence of reflux oesophagitis.
The average age of the patient cohort was 52 years and the sex distribution was 43 males and 57 females. The symptom duration ranged from 3 months to 33 years.
Type II achalasia was the commonest in this patient cohort however several patients did not fall clearly into the defined categories. In patients with recurrent symptoms it was not always possible to determine the original classification. The distribution is shown in Table 1.
Table 1
| Chicago Classification | N |
|---|---|
| Type I | 16 |
| Type II | 58 |
| Type III | 14 |
| Variant | 4 |
| Not specified | 8 |
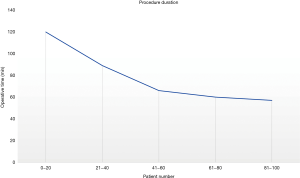
The overall average operative time was 78 min, however the introduction of this procedure has shown a clearly defined learning curve (Figure 6) and this is seen in the progressive reduction in operative times down to an average of 57 min in the last 20 cases in the series. The procedure time for cases 1–20 was 120 min, 21–40 was 89 min, 41–60 was 66 min and 61–80 was 60 min.The mean myotomy length was 9.2 cm and the range was 4 to 13 cm. The myotomy mean length according to type of achalasia is shown in the Table 2.
Table 2
| Chicago Classification | Mean myotomy length (cm) |
|---|---|
| Type I | 8.5 |
| Type II | 9.4 |
| Type III | 9.4 |
| Overall mean [range] | 9.2 [4–13] |
In several of the revisional cases the myotomy was quite short as the only problem related to an incomplete myotomy of the LES and this short myotomy resulted in relief of symptoms.
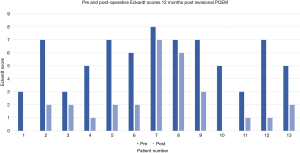
Follow-up data was available for 54 of the 80 patients (67.5%) that had reached 12 months post-POEM. The average Eckardt score fell from 6.85 to 1.68. Early follow-up showed a drop in the Eckardt score to 3 or less representing a successful outcome in 92% of patients.
There were two aborted primary procedures, one who had a previous perforation as a result of a pneumatic dilatation and one who had long-standing achalasia with a very dilated oesophagus and multiple previous dilatations. With more experience, patients who had previously been treated with LHM or POEM and had recurrent symptoms underwent revisional POEM.
Twenty-two revisional procedures were undertaken. The distribution related to Chicago Classification is shown in Table 3. The average pre-operative Eckardt score in this group was 6.25 and this fell to 2.36 post-POEM. Two patients did not improve significantly post-POEM in the revisional group. This equated to a 91% success rate in the revisional group (Figure 7).
Table 3
| Type | Variant | Type I | Type II | Type III | Total |
|---|---|---|---|---|---|
| LHM | 3 | 7 | 3 | 4 | 17 |
| Poem | 3 | 1 | 0 | 0 | 4 |
| Pneumatic dilatation* | – | – | – | – | 1 |
*, the original classification of the pneumatic perforation is unknown.
Discussion
The results of this first series from Australia is comparable to the experience in the literature. A systematic review on the long-term outcomes of POEM has not been published to-date. Most studies report on relatively short follow-up periods, preventing the assessment of long-term safety and efficacy of POEM. The following ten studies were identified to report on outcomes ≥2 years following the procedure (Table 4).
Table 4
| Studies | Number of patients | Length of myotomy (cm) | Complications | Eckardt score ≤3 at 2-year F/U | GORD |
|---|---|---|---|---|---|
| Chen |
45 | 9.56 (±1.5) | 5/45 (11.11%) | 100% | 6.67% |
| Inoue |
500 to start; 370 at 1–2 years; 61 at 3 years | 11 [9–13] | 3.2% | 91% (88.5% at 3 years) | 21.3% |
| Werner |
80 | 11.3 [5–18] | No major AE 16/80 (20%) | 78.5%; when learning curve cases excluded—91.5% | 17.8% (req. daily PPI consumption) |
| Hungness |
103 | 10.7 (±3) | 19/103 (18.4%) | 93.2% | 28% |
| Zhang |
32 | 8.2 [3–15] | 6/32 (18.8%) | 90.6% | 18.8% |
| Nabi |
408 to start; 172 at 2 years; 51 at 3 years | 10 [3–18] | 36% | 91% at 2 years; 90.2% at 3 years | 28.3% |
| Guo |
67 | Abstract only | Abstract only | 88% at 3 years | 13.4% |
| Teitelbaum |
23 | Not reported | 1/36 (2.8%) | 83% at 5 years | 39% |
| Li |
564 to start; 358 1–2 years; 357 2–3 years; 237 3–4 years; 48 4–5 years | 8 [3-13] | Major AE 36/564 (6.4%) | 92.2% at 1–2 years; 91.1% at 2–3 years; 88.6% at 3–4 years; 87.1% at 4–5 years | 36.5% |
| Werner |
112 | Not reported | Serious AE 2.7% | 83% | 44% |
F/U, follow-up; GORD, gastro-oesophageal reflux disease; AE, adverse event; PPI, proton pump inhibitor.
In each study, treatment success is defined as a post-procedure Eckardt score of 3 or less. These studies demonstrate excellent long-term efficacy of 83–100% treatment success at 2 years. One study reported 87.1% treatment success at 5 years in 48 patients. Notably, there is loss to follow-up in many of the reported studies, leading to an inherent selection bias.
Controversies in POEM
Gastro-oesophageal reflux disease (GORD) post-POEM
Gastro-oesophageal reflux is the most common adverse event following a POEM procedure. Rates vary significantly between studies. In part, this heterogeneity may be explained by differing evaluations: symptomatic reflux vs. endoscopic evidence of reflux oesophagitis. Furthermore, the duration of follow-up may also affect rates of reflux, with incidence decreasing with increasing time of follow-up. In Shiwaku’s study of 1,176 patients, endoscopic examination was undertaken within 6 months of the procedure to assess for erosive oesophagitis (6). Symptomatic GORD was observed in 14.8% of patients, while 63% demonstrated some degree of erosive oesophagitis. Only 6.2% demonstrated severe erosive oesophagitis with Los Angeles classification Grade C or D. Patients were treated with a proton pump inhibitor (PPI). None of these patients suffered from refractory GORD requiring fundoplication. In contrast LHM has often been combined with an anti-reflux procedure to reduce reflux rates and reportedly drops the rate from 41.5% to 14.5% (21-23).
A systematic review and meta-analysis by Repici et al. described a significantly greater incidence of reflux disease in patients following POEM when compared to those who underwent LHM with fundoplication (24). In this analysis of 45 studies and 4,123 patients, symptomatic GORD rates were 19% following POEM and 8.8% following LHM with fundoplication. Rates of oesophagitis were 29.4% after POEM and 7.6% after LHM with fundoplication. However, this study concedes that reflux rates were lower amongst studies with a longer follow-up duration. Mean follow-up among POEM patients was 9.3 months (range, 2–30 months) while follow-up among patients who underwent LHM fundoplication was 26.6 months (range, 12–49 months).
A subsequent systematic review by Zaninotto et al., described rates of post-POEM endoscopic oesophagitis between 17% and 59.2% (25). This study included the analysis done by Repici et al., with a total of 2,544 patients who underwent POEM. Once again, there was heterogeneity in duration of follow-up among patients studied.
A randomised trial by Werner et al., published in 2019 compared PPI use, reflux rates and diagnosis of oesophagitis between 112 patients who underwent POEM and 109 patients who underwent LHM and Dor fundoplication (21). At 3-month follow-up, 57% of patients who underwent POEM and 20% of those who underwent LHM had evidence of reflux oesophagitis on gastroscopy. This reduced to 44% of those who underwent POEM and 29% of those who underwent LHM at 2-year follow-up. The study demonstrated no significant difference at 2-year follow-up in rates of reflux oesophagitis between patients who underwent POEM and those who underwent LHM and Dor fundoplication.
The American Gastroenterological Association recommends medical practitioners to clearly state the risk of developing reflux post-POEM with post-procedure management including:
- Objective testing for oesophageal acid exposure;
- Long-term and possible lifelong PPI use;
- Surveillance for long-term consequences of GORD with annual upper endoscopy.
These findings, recommendations and patient reluctance to commit to long-term PPI use, have inspired consideration of an anti-reflux procedure to be considered with POEM.
An area for consideration is the use of POEM in younger patients. Most published studies identify reflux after POEM as being significant in over 50% of patients as there is no antireflux component to this procedure (8). Prolonged exposure of the oesophageal lining to acid may result in Barrett’s change with the subsequent risk of oesophageal cancer. It may be more appropriate to use a LHM with an antireflux component in this group. In our experience, patients frequently have evidence of reflux on endoscopy post POEM but do not have symptoms commensurate with their degree of reflux.
Type III achalasia
POEM procedure is emerging as the first-line treatment for type III achalasia. This is due to the ability to perform a longer myotomy and therefore achieve improved symptom control with respect to pain in this often treatment resistant patient population.
A meta-analysis of 20 studies (1,575 patients) by Andolfi and Fisichella (2019) compared clinical outcomes of patients with achalasia after botulinum toxin injection, pneumatic dilatation, LHM and POEM based on manometric subtypes (26). The analysis showed significantly better rates of treatment success with POEM when compared to LHM in type I and III achalasia, with equivalent success rates in type II achalasia.
In type I achalasia, overall treatment success following LHM was 81%, while in POEM it was 95% (P=0.032). In type III achalasia, 71% treatment success was demonstrated with LHM when compared to 93% treatment success following POEM.
Whilst there is the ability to undertake a longer myotomy for type III achalasia patients this does carry a long-term risk of gross oesophageal dilatation and complete functional failure and so we would caution the use of excessively long myotomies.
Conclusions
POEM is now an established treatment for achalasia with outcomes that are at least as good if not better than LHM. POEM has been particularly useful in the treatment of type III achalasia as it allows the length of the myotomy to be varied. Reflux is the main issue that is associated with POEM that is significantly higher in this group and may have long term consequences of Barrett’s oesophagus. The first Australian series presented confirms that POEM is an effective treatment for the management of all types of achalasia and is safe. Future studies should be directed to evaluating longer term outcomes and potential complications related to reflux.
Acknowledgments
The main author gratefully acknowledges the assistance provided by Professor Karl Fuchs during the introduction of POEM in Australia.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Sarah Thompson) for the series “Achalasia” published in Annals of Esophagus. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoe.2020.03.01). The series “Achalasia” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The institutional ethical approval and individual consent for this retrospective analysis were waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sadowski DC, Ackah F, Jiang B, et al. Achalasia: incidence, prevalence and survival. A population-based study. Neurogastroenterol Motil 2010;22:e256-61. [Crossref] [PubMed]
- Duffield JA, Hamer PW, Heddle R, et al. Incidence of Achalasia in South Australia Based on Esophageal Manometry Findings. Clin Gastroenterol Hepatol 2017;15:360-5. [Crossref] [PubMed]
- Ortega JA, Madureri V, Perez L. Endoscopic myotomy in the treatment of achalasia. Gastrointest Endosc 1980;26:8-10. [Crossref] [PubMed]
- Pasricha PJ, Hawari R, Ahmed I, et al. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy 2007;39:761-4. [Crossref] [PubMed]
- Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophagal achalasia. Endoscopy 2010;42:265-71. [Crossref] [PubMed]
- Shiwaku H, Inoue H, Onimaru M, et al. Multicenter collaborative retrospective evaluation of peroral endoscopic myotomy for esophgeal achalasia: analysis of data from more than 1300 patients at eight facilities in Japan. Surg Endosc 2020;34:464-8. [Crossref] [PubMed]
- Ahmed Y, Othman MO. Peroral endoscopic myotomy (POEM) for achalasia. J Thorac Dis 2019;11:S1618-28. [Crossref] [PubMed]
- Hamer PW, Holloway RH, Crosthwaite G, et al. Update in achalasia: what the surgeon needs to know. ANZ J Surg 2016;86:555-9. [Crossref] [PubMed]
- Eckardt VF. Clinical presentations and complications of achalasia. Gastrointest Endosc Clin N Am 2001;11:281. [Crossref] [PubMed]
- Rohof WOA, Bredenoord AJ. Chicago Classification of Esophageal Motility Disorders: Lessons Learned. Curr Gastroenterol Rep 2017;19:37. [Crossref] [PubMed]
- Oelschlager BK, Chang L, Pellegrini CA. Improved outcome after extended gastric myotomy for achalasia. Arch Surg 2003;138:490-5; discussion 495-7. [Crossref] [PubMed]
- Chen X, Li QP, Ji GZ, et al. Two-year follow-up for 45 patients with achalasia who underwent peroral endoscopic myotomy. Eur J Cardiothorac Surg 2015;47:890-6. [Crossref] [PubMed]
- Inoue H, Sato H, Ikeda H, et al. Per-Oral Endoscopic Myotomy: A Series of 500 Patients. J Am Coll Surg 2015;221:256-64. [Crossref] [PubMed]
- Werner YB, Costamagna G, Swanström LL, et al. Clinical response to peroral endoscopic myotomy in patients with idiopathic achalasia at a minimum follow-up of 2 years. Gut 2016;65:899-906. [Crossref] [PubMed]
- Hungness ES, Sternbach JM, Teitelbaum EN, et al. Per-oral Endoscopic Myotomy (POEM) After the Learning Curve: Durable Long-term Results With a Low Complication Rate. Ann Surg 2016;264:508-17. [Crossref] [PubMed]
- Zhang W, Linghu EQ. Peroral Endoscopic Myotomy for Type III Achalasia of Chicago Classification: Outcomes with a Minimum Follow-Up of 24 Months. J Gastrointest Surg 2017;21:785-91. [Crossref] [PubMed]
- Nabi Z, Ramchandani M, Chavan R, et al. Per-oral endoscopic myotomy for achalasia cardia: outcomes in over 400 consecutive patients. Endosc Int Open 2017;5:E331-9. [Crossref] [PubMed]
- Guo H, Yang H, Zhang X, et al. Long-term outcomes of peroral endoscopic myotomy for patients with achalasia: a retrospective single-center study. Dis Esophagus. 2017;30:1-6. [Crossref] [PubMed]
- Teitelbaum EN, Dunst CM, Reavis KM, et al. Clinical outcomes five years after POEM for treatment of primary esophageal motility disorders. Surg Endosc 2018;32:421-7. [Crossref] [PubMed]
- Li QL, Wu QN, Zhang XC, et al. Outcomes of per-oral endoscopic myotomy for treatment of esophageal achalasia with a median follow-up of 49 months. Gastrointest Endosc 2018;87:1405-1412.e3. [Crossref] [PubMed]
- Werner YB, Hakanson B, Martinek J, et al. Endoscopic or Surgical Myotomy in Patients with Idiopathic Achalasia. N Engl J Med 2019;381:2219-29. [Crossref] [PubMed]
- Campos GM, Vittinghoff E, Rabl C, et al. Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg 2009;249:45-57. [Crossref] [PubMed]
- Stefanidis D, Richardson W, Farrell TM, et al. Guidelines for the surgical treatment of oesophageal achalasia. Surg Endosc 2012;26:296-311. [Crossref] [PubMed]
- Repici A, Fuccio L, Maselli R, et al. GERD after per-oral endoscopic myotomy as compared with Heller's myotomy with fundoplication: a systematic review with meta-analysis. Gastrointest Endosc 2018;87:934-943.e18. [Crossref] [PubMed]
- Zaninotto G, Leusink A, Markar SR. Management of achalasia in 2019. Curr Opin Gastroenterol 2019; [Epub ahead of print]. [Crossref] [PubMed]
- Andolfi C, Fisichella PM. Meta-analysis of clinical outcome after treatment for achalasia based on manometric subtypes. Br J Surg 2019;106:332-41. [Crossref] [PubMed]
Cite this article as: Crosthwaite GL, Sejka M. Per-oral endoscopic myotomy (POEM): overview and experience of 100 cases by a single surgeon in Australia. Ann Esophagus 2020;3:12.