A case of long-term survival of primary malignant melanoma of the esophagus after surgery and a review of the literature
Introduction
Primary malignant melanoma of the esophagus (PMME) is a very rare tumor occurs mostly in 60–70 years old male patients (1). PMME often presents as polypoid lesion in esophagus and the most common symptoms includes dysphagia, retrosternal or epigastric discomfort or pain or weight loss (1). With the development of technology of diagnosis, more and more PMME has been diagnosed in recent years. However, the prognosis of PMME is yet not encouraging due to the high potential of metastasis (1). Like most other malignant tumors, early diagnosis and treatment can significantly improve the prognosis of these patients (2). Image examination including upper gastrointestinal series and computed tomography (CT) are very useful for clinical staging. Positive expression of S100 protein, HMB45 and neuron-specific enolase from pathologic and immunohistochemical is helpful for definitive diagnosis of PMME (3). Eight years ago, we encountered a case of PMME in endoscopy and diagnosed it by pathology. We follow up the case until now and find that the patient is still alive.
Case presentation
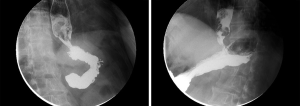
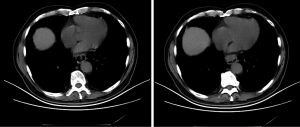
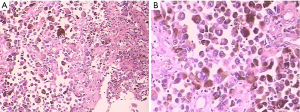
A 75-year-old man came to our institute for an examination in November 23, 2010 due to difficulty in swallowing for about one month. The symptom is getting worse when eating solid foods. Upper gastrointestinal endoscopy showed a dark brown mass (3 cm × 2 cm) in the esophagus 34–39 cm from the incisors. Microscopic examination revealed variously pigmented unusual cells were observed in the tumor. A circular filling defect in the lower esophagus was observed in upper gastrointestinal series (Figure 1). CT scan of the chest and upper abdomen revealed the esophagus wall was thicker than normal situation (Figure 2). PMME was suspected in this case and further examination was performed. The PET-CT examination did not find any proof of tumor metastasis and skin examination did not find any proof of melanoma. A subtotal esophagectomy was performed using the Sweet technique in December 1, 2010. Gross specimen showed a dark brown mass measuring 3 cm × 2 cm located in the lower part of esophagus. Postoperative pathological diagnosis was PMME and tumor invaded the submucosa of the esophagus, all the detectable lymph nodes (fifteen lymph nodes) are negative and the esophageal margin was free from tumors (Figure 3). The patient did not receive any further treatment due to his poor physical situation and early pathological stage. We have followed up the patient until now, the patient is still healthy currently, no tumor metastasis and recurrence signs have been seen.
Discussion
PMME is very rare tumor only representing 0.1% to 0.2% of all esophageal malignancies and 0.5% of noncutaneous melanomas are detected in esophagus. It occurs mostly in 60–70 years old male patients, only few younger patients have been reported (1).
Baur et al. reported the first case of PMME in 1906 (4). Garfinkle and Cahan confirmed the first diagnosis of PMME with histological evidence in 1952 (5). There were only 337 cases had been reported throughout the world by 2011 (6). PMME often presents as polypoid lesion and the most common symptoms includes dysphagia, retrosternal or epigastric discomfort or pain or weight loss (1). Most of PMME are distributed in the middle-lower part of the esophagus (7). With the development of technology of diagnosis, more and more PMME has been diagnosed in recent years. Examinations including chest and upper abdominal CT, barium swallow, EUS and fluorodeoxyglucose positron-emission tomography (FDG-PET) are useful for clinical staging (8,9). FDG-PET is very sensitive in detecting lymph node metastases (2), so it is necessary to perform FDG-PET when lymph node metastases were suspected. Positive expression of S100 protein, HMB45 and neuron-specific enolase in pathologic and immunohistochemical examination is essential for pathologic diagnosis of PMME (10).
The prognosis of PMME is not encouraging due to its high potential of metastasis (11). The average survival period of PMME after diagnosis is about 10–14 months, with a 5-year survival rate of 4.2% (1). Wang et al. showed that none of patients with tumor later than stage Ib had survived longer than 5 years in their study (12). Only a few cases of survival time amount to 5 years after operation were reported (3,8,9,12-20). The characteristics of all included patients were listed in Table 1. All included patients underwent esophagectomy and several patients received adjuvant treatment, which includes chemotherapy, radiotherapy, radiochemotherapy and immune hormone therapy. One patient was treated with radiochemotherapy 30 months after surgery due to metastasis to a supraclavicular lymph node was found (3). The patient had survived at least 9 years after operation, which suggested that radiochemotherapy might be an effective therapy when distant metastasis was found after surgery. Most patients with tumor later than stage Ib received adjuvant therapy. However, two patients with tumor later than stage Ib also obtained long-term survival without adjuvant therapy (14,20). So the effectiveness of adjuvant therapy for patient with tumor later than stage Ib may be still controversial.
Table 1
| Case No. | Author | Year | Age (year) | Sex | Stagea | Treatment | Survival |
|---|---|---|---|---|---|---|---|
| 1 | Khoury-Helou |
2001 | 64 | Female | T1bN0M0 | Subtotal esophagectomy + radiochemotherapy | 9 y |
| 2 | Kawada |
2007 | 64 | Female | T2N0M1a | Pre- and post-hormone chemotherapy + immunohormone therapy + subtotal esophagectomy | 7 y |
| 3 | Gupta |
2009 | 55 | Male | T3N2M0 | esophagectomy + postoperative adjuvant chemotherapy | 69 m |
| 4 | Wang |
2013 | 62 | Male | 0 | Esophagectomy | 94 m |
| 5 | Wang |
2013 | 67 | Male | IA | Esophagectomy | 114 m |
| 6 | Suzuki |
1980 | NR | NR | NR | Surgery | 10 y |
| 7 | Hamdy |
1991 | 40 | Female | T1bN+M0b | Subtotal esophagectomy | 12 y |
| 8 | De Mik |
1992 | 75 | Male | T1bN0M0 | Esophageal resection | 5 y |
| 9 | Suehs |
1961 | 48 | Female | T1bN0M0 | Subtotal esophagectomy | 6 y 6 m |
| 10 | Itami |
2004 | 52 | Female | T2N0M0 | Neoadjuvant chemotherapy + adjuvant cisplatin + subtotal esophagectomy | 11 y |
| 11 | Uetsuka |
2004 | 45 | Male | T1bN+M0b | Pre- and post-hormone chemotherapy + immunohormone therapy + sub-total esophagectomy | 7 y 4 m |
| 12 | Li |
2007 | 46 | Female | T2N0M0 | Radiotherapy + esophagectomy | 17 y |
| 13 | Sabat |
2015 | 38 | Male | T3N1M0 | Esophagectomy | 7 y |
a, according to the 7th edition of International Union Against Cancer (UICC) TNM staging system for esophageal cancers; b, metastatic lymph nodes were observed while the number of metastatic lymph nodes was not given in these articles. NR, not reported.
The prognosis of melanoma has changed over past few years. Immunotherapy is becoming more and more promising in treating patients with advanced melanoma. Agents targeting the programmed death-1 (PD-1) receptor and its ligand (PD-L1) are hopeful treatment for advanced melanoma nowadays (21,22). Nivolumab is being developed to treat above disease and many other malignancies with promising results. Several trials have showed encouraging effect in advanced melanoma and non-small-cell lung cancer with a tolerable toxicity profile (23), which may provide a new approach to the treatment of PMME. Vaccines, cytokines (IL-2) have also been used for the clinical treatment of melanoma (24). Zheng et al. reported two patients underwent postoperative radiotherapy and chemotherapy and immunotherapy had longer disease-free survival than patient underwent postoperative radiotherapy and chemotherapy (25), which indicated immunotherapy may contribute to the better disease-free survival.
To sum up, PMME is a rare disease with dreadful prognosis. In this article, we presented a case of PMEE with long term survival after surgery. By review the previous cases of PMME with long-term survival, we found surgery is standard, and only treatment that can offer the opportunity for long-term survival. When distant metastasis occurs, radiochemotherapy might be an effective therapy to prolong survival. Immunotherapy is a promising therapy and may result in better disease-free survival.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoe.2019.03.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sabanathan S, Eng J, Pradhan GN. Primary malignant melanoma of the esophagus. Am J Gastroenterol 1989;84:1475-81. [PubMed]
- Crippa F, Leutner M, Belli F, et al. Which kinds of lymph node metastases can FDG PET detect? A clinical study in melanoma. J Nucl Med 2000;41:1491-4. [PubMed]
- Khoury-Helou A, Lozac'h C, Vandenbrouke F, et al. Primary malignant melanoma of the esophagus. Ann Chir 2001;126:557-60. [Crossref] [PubMed]
- Baur EH, von Fall E. Primaerem Melanoma de Oesophagus. Arb Geb Pathol Anat Inst Tuebingen 1906;5:343-54.
- Garfinkle JM, Cahan WG. Primary melanocarcinoma of the esophagus; fist histologically proved case. Cancer 1952;5:921-6. [Crossref] [PubMed]
- Bisceglia M, Perri F, Tucci A, et al. Primary malignant melanoma of the esophagus: a clinicopathologic study of a case with comprehensive literature review. Adv Anat Pathol 2011;18:235-52. [Crossref] [PubMed]
- Sanchez AA, Wu TT, Prieto VG, et al. Comparison of primary and metastatic malignant melanoma of the esophagus: clinicopathologic review of 10 cases. Arch Pathol Lab Med 2008;132:1623-9. [PubMed]
- Kawada K, Kawano T, Nagai K, et al. Local injection of interferon beta in malignant melanoma of the esophagus as adjuvant of systemic pre- and postoperative DAV chemotherapy: case report with 7 years of long-term survival. Gastrointest Endosc 2007;66:408-10. [Crossref] [PubMed]
- Gupta V, Kochhar R, Sinha SK, et al. Primary malignant melanoma of the esophagus: long-term survival after radical resection. J Thorac Oncol 2009;4:1180-2. [Crossref] [PubMed]
- Joob AW, Haines GK, Kies MS, et al. Primary malignant melanoma of the esophagus. Ann Thorac Surg 1995;60:217-22. [Crossref] [PubMed]
- Chalkiadakis G, Wihlm JM, Morand G, et al. Primary malignant melanoma of the esophagus. Ann Thorac Surg 1985;39:472-75. [Crossref] [PubMed]
- Wang S, Tachimori Y, Hokamura N, et al. Diagnosis and surgical outcomes for primary malignant melanoma of the esophagus: a single-center experience. Ann Thorac Surg 2013;96:1002-6. [Crossref] [PubMed]
- Suzuki H, Nagayo T. Primary tumors of the esophagus other than squamous cell carcinoma--histologic classification and statistics in the surgical and autopsied materials in Japan. Int Adv Surg Oncol 1980;3:73-109. [PubMed]
- Hamdy FC, Smith JH, Kennedy A, et al. Long survival after excision of a primary malignant melanoma of the oesophagus. Thorax 1991;46:397-8. [Crossref] [PubMed]
- De Mik JI, Kooijman CD, Hoekstra JB, et al. Primary malignant melanoma of the oesophagus. Histopathology 1992;20:77-9. [Crossref] [PubMed]
- Suehs OW. Malignant melanoma of the esophagus. Ann Otol Rhinol Laryngol 1961;70:1140-7. [Crossref] [PubMed]
- Itami A, Makino T, Shimada Y, et al. A case of primary malignant melanoma of the esophagus with long term survival. Esophagus 2004;1:135-7. [Crossref]
- Uetsuka H, Naomoto Y, Fujiwara T, et al. Primary malignant melanoma of the esophagus: long-term survival following pre- and postoperative adjuvant hormone/chemotherapy. Dig Dis Sci 2004;49:1646-51. [Crossref] [PubMed]
- Li B, Lei W, Shao K, et al. Characteristics and prognosis of primary malignant melanoma of the esophagus. Melanoma Res 2007;17:239-42. [Crossref] [PubMed]
- Sabat J, Mannan R, Legasto A, et al. Long-term survivor of primary malignant melanoma of the esophagus treated with surgical resection. Int J Surg Case Rep 2015;6C:182-5. [Crossref] [PubMed]
- Hirano F, Kaneko K, Tamura H, et al. Blockade of B7-H1 and PD-1 by monoclonal antibodies potentiates cancer therapeutic immunity. Cancer Res 2005;65:1089-96. [PubMed]
- Ott PA, Hodi FS, Robert C. CTLA-4 and PD-1/PD-L1 blockade: new immunotherapeutic modalities with durable clinical benefit in melanoma patients. Clin Cancer Res 2013;19:5300-9. [Crossref] [PubMed]
- Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med 2012;366:2443-54. [Crossref] [PubMed]
- Schwartzentruber DJ, Lawson DH, Richards JM, et al. gp100 peptide vaccine and interleukin-2 in patients with advanced melanoma. N Engl J Med 2011;364:2119-27. [Crossref] [PubMed]
- Zheng J, Mo H, Ma S, et al. Clinicopathological findings of primary esophageal malignant melanoma: report of six cases and review of literature. Int J Clin Exp Pathol 2014;7:7230-5. [PubMed]
Cite this article as: Zhao W, Guo X, Yang Y. A case of long-term survival of primary malignant melanoma of the esophagus after surgery and a review of the literature. Ann Esophagus 2019;2:4.