
Hybrid approaches to minimally invasive esophagectomy
Introduction
The specificity of esophagectomy techniques stands in the necessity to have two-field or three-field surgical approaches to perform the oncological resection and the reconstruction. At the current time, esophagectomy is performed mostly in tertiary centers because of its complexity. With the progress of anaesthesiology, instrumentations and surgical skills, the possibility to reduce the surgical trauma has grown up since the 90’s. Since the last two decades, the global preference for smaller incisions and minimally invasive approaches in the field of esophageal surgery has become a reality worldwide (1-3). Moreover, this trend is progressively supported by level-one evidences in the literature review, with to date, three prospective and randomized clinical trials demonstrating the benefits of such approaches, even after neoadjuvant treatment (4-6). However, the major issue with minimally invasive esophagectomy (MIE) lays in the gastric reconstruction and the confection of the anastomosis. For these reasons, many surgeons remain unsatisfactory with the anastomosis confection using minimally invasive techniques. As a result, many of them have opted for a combination of mixed conventional and minimally invasive approaches to overcome this issue and to conserve the benefits of minimally invasive surgery (7,8).
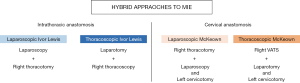
The hybrid approaches to MIE are the combination of minimally invasive approaches mixed to open approaches by applying the minimally invasive techniques at one level of the two stages (abdomen or thorax) of the procedure. This can be at the level of the abdominal phase using a laparoscopy or at the thoracic phase by using a video-assisted thoracoscopic surgery (VATS). The hybrid techniques can be clearly decided prior to surgery in the surgical decision-making strategy to focus and to keep conventional surgery for one the two stages because of expected issues. Furthermore, decision to opt for hybrid techniques can also result from the necessity to convert intraoperatively at both stages of the technique during total MIE and to conserve the benefits of MIE for the remaining procedure.
The most described and studied of these hybrid techniques are is represented by the laparoscopic hybrid Ivor Lewis esophagectomy where the gastric mobilization is performed laparoscopically whereas the confection of the intrathoracic anastomosis is performed with a standard fashion. This technique is specifically indicated for adenocarcinoma of the gastro-esophageal junction (GEJ) or for tumor of the lower third esophagus. In addition, the hybrid VATS esophagectomy combined with laparotomy has been described but data on this technique are scarce.
The goal of this review is to depict the several techniques of hybrid esophagectomy and to discuss the results of such techniques.
Surgical techniques
The several hybrid approaches to MIE avec summarized in Figure 1 with the different levels of anastomosis.
Laparoscopic hybrid Ivor Lewis esophagectomy
The hybrid laparoscopic Ivor Lewis esophagectomy combines an abdominal laparoscopic approach for gastric mobilization and keeps a right thoracotomy for oncological transthoracic en-bloc esophagectomy with intrathoracic anastomosis. The laparoscopy is performed with CO2 pneumoperitoneum insufflation with a patient in reverse Trendelenburg with a supine split-leg position (French position). The technique required mostly 5 ports (usually 2 ports of 5 mm, 2 of 11 mm and one of 12). Gastric mobilization is performed as an open procedure consisting in division of the gastro-hepatic ligament and the greater omentum until the short gastric vessels are reached. The greater omentum is completely divided keeping intact the right gastroepiploic vessels. The dissection is easily performed using ultrasonic energy (Harmonic scalpel®). The left gastric vessels are dissected and divided at the superior part of the pancreatic gland. Division is performed using clips or vascular automatic stapler. A radical abdominal lymph node dissection is performed according to the definition of standard D2-lymphadenectomy (celiac axis, splenic, left common hepatic and left gastric lymph node stations). An incomplete wide 4-cm gastric tubulization is obtained by stapling the lesser curvature of the stomach parallel to the right gastro-epiploic artery (SC45 A Echelon Flex Endopath Stapler®, reload 45 mm Gold). The tubulization is initiated at the abdominal phase and will be ended in the thorax. The integrity of the vascularization and the viability assessment of the gastric tube can be checked using the indocyanine green (ICG) fluorescence imaging. A laparoscopic feeding-jejunostomy is usually added at the end of the procedure. No abdominal drainage is required. The patient is then turned to the left lateral decubitus position. A right posterolateral thoracotomy is then performed requiring contralateral single-lung ventilation using a left double-lumen tube (or an endobronchial blocker in case of failure). En-bloc esophagectomy is performed through a standard fashion after division of the azygos arch. A radical and standardized mediastinal lymphadenectomy is performed including several lymph nodes stations whatever the histological subtype: subcarinal, right and left latero-tracheal, paraesophageal and thoracic duct. The end to side intrathoracic anastomosis can be performed through different techniques depending of the surgeons convictions: hand-sewn, mechanical (25 mm echelon automatic circular powered) or semi-automatic. The anastomotic integrity is checked using a methylene blue test in the nasogastric tube. Two perianastomotic chest-tubes are let in place.
Thoracoscopic Ivor Lewis esophagectomy
The hybrid thoracoscopic Ivor Lewis esophagectomy combines an abdominal laparotomy approach for gastric mobilization and keeps a right VATS for oncological transthoracic en-bloc esophagectomy. The intrathoracic anastomosis is performed under thoracoscopy. At the current time, this technique has been abandoned because the difficult part lies in the confection of the anastomosis. This technique is now replaced by total MIE Ivor Lewis (VATS or robotic).
Hybrid McKeown esophagectomy
McKeown esophagectomy consists in a 3-field procedure with a cervical gastric reconstruction. In this setting the minimally approaches can be mixed to open approaches by applying the minimally invasive techniques either for the abdominal stage (laparoscopy) or for the thoracic stage by VATS. Hybrid McKeown can result also from a total MIE requiring conversion at both stages of the procedure.
Laparoscopic McKeown esophagectomy
The indications of such technique are when a troublesome dissection is expected into the chest, leading to consider a first-line thoracotomy. A minimally invasive approach is kept for the abdominal stage. This can be the case after high dose of radiation in the chest, after previous chest surgery, in case of a bulky tumor or in case of an associated pulmonary or mediastinal resection. The technique begins with a right posterolateral thoracotomy for esophageal mobilization and lymphadenectomy in a standard fashion. After completion of the thoracic stage, the patient is turned and positioned in a supine split-leg position (French position) with a left arm along the body to allow a left cervical incision. The laparoscopic abdominal stage is strictly identical as described above. The gastric mobilization and lymphadenectomy is performed in an usual way using CO2 insufflation. The gastric tubulization is initiated 2-cm before the pylorus in order to obtain a long 4-cm wide gastric tube to reach the neck. The tubulization is performed intra-corporeally and completed under laparoscopy using almost 8 or 9 reloads of automatic stapler (45 Gold Echelon®). Then the gastric tube is attached to the resected specimen at the level of the GEJ in the hiatus with two stitches. Under laparoscopic vision, the resected specimen and the gastric tube are gently pulled-up to the left cervical incision though the posteris or mediastinum. The resected specimen is then removed through the cervicotomy. The anastomosis in then performed end-to-side or side-to-side by hand-sewn fashion or by semi-mechanical techniques. An alternative possibility is to fashion the gastric conduit extra-corporeally through a 5 cm midline laparotomy incision secured with an Alexis wound retractor. This option required to have previously positioned a tutor in the posterior mediastinum (nasogastric tube or a chest-tube) to pull the gastric tube to the neck. The resected specimen is then removed through the minilaparotomy. The gastric tube is then stitched to the tutor and gently pulled-up to the neck incision through the posterior mediastinum under laparoscopic vision.
VATS McKeown esophagectomy
The indications of such technique are when a difficult dissection is expected into the abdomen leading to consider a laparotomy. A VATS esophageal mobilization is normally performed before the laparotomy. This can be the case after high dose of radiation in the abdomen, after previous abdominal surgery, in case of a bulky tumor invading the diaphragm or the pancreatic gland, in case of associated abdominal resection or when a different route is considered for the gastric tube reconstruction (pre or retrosternal). For note, the hybrid VATS esophagectomy can also be indicated when another substitute than the stomach is considered requiring laparotomy (colonic interposition). The technique begins with the thoracoscopic esophageal mobilization (9,10). The patient can be positioned in prone position but also in left-lateral decubitus. Each position has some advantages and disadvantages. Prone position does not require double-lumen. The patient is positioned in prone position with a single-lumen tube and the right lung is collapsed by CO2 insufflation (8 mmHg). The disadvantages of prone position are the difficulty to turn the patient and a poor exposure in case of intraoperative conversion. Three or 4 ports are required generally (4th, 6th and 8th intercostal space). Esophageal mobilization is performed through a standardized technique consisting in pleural opening, division of azygos vein, en-bloc esophageal dissection and mediastinal lymphadenectomy. The dissection is made easier using the “suspension” technique using a Penrose drain around the esophagus. Thoracic duct is ligated at the base of the thorax. The esophagus is not transected to allow the digestive continuity and the gastric pull-up to the neck at the second step of the procedure. A perianastomotic chest-tube is let in place. Then the patient is turned supine. A median laparotomy and left cervical incision are performed through a standard fashion. The gastric tubulization is performed and the gastric tube is pulled-up to the neck through the posterior mediastinum. It is also possible in this technique to use the retrosternal route if needed.
Results of hybrid esophagectomy
Hybrid esophagectomy including laparoscopy
Even if several techniques of hybrid esophagectomy procedures have been described (2), the best knowledge to date come from the hybrid Ivor Lewis operation (5,7,11-15). The concept of a laparoscopic approach for gastric mobilization comes from the hypothesis that the laparoscopy would have the potential to significantly decrease the respiratory consequences when compared to a conventional laparotomy. This assumption was argued by the results of laparoscopic approach in others indications such as cholecystectomy for example (16-19). The post-laparotomy diaphragmatic dysfunction, the immunological stress and the impairment of the respiratory function have been suggested as consequences of conventional laparotomy. In this setting, the laparoscopic approach has indubitably several advantages over the conventional laparotomy. Advantages can be summarized as follow: exploration of peritoneal cavity to rule out carcinomatosis and unnecessary laparotomy, standardization of the gastric mobilization, reduction of blood loss, possibility to ligate easily both left and short gastric vessels, good exposure whatever the patient’s weigh and especially in overweighed patients, excellent visibility with magnification to perform radical lymphadenectomy, possibility to add a feeding jejunostomy if needed and at last allow the inclusion in an enhanced recovery after surgery (ERAS) program. In addition, all the abdominal part of the laparoscopic procedure seems easier to teach than a VATS approach. At last, this approach seems more attractive because the confection of the intrathoracic anastomosis is performed with an open approach making it easier compared to all the MIE techniques of anastomosis (20). This represents a strong argument for surgeons who have already faced problems in the confection of the anastomosis with VATS.
Majority of available literature of hybrid laparoscopic Ivor Lewis procedure come from non-controlled studies comparing such techniques with open conventional procedure. Very recently, the results of the French randomized MIRO trial have brought good informations regarding short, mid and long-term outcomes of laparoscopic hybrid Ivor Lewis procedure (5). The first and easiest point to be demonstrated was the beneficial effect of laparoscopy on 30-day major pulmonary complications (15% for laparoscopy vs. 42% for laparotomy) (7). This decrease was also confirmed by further studies (12-14). The second point demonstrated with laparoscopy was the substantial effect on postoperative mortality. Based on propensity-score matching study, a retrospective large nationwide study, including more than three thousand patients over two years, found a significant reduction in 30- and 90-day mortality rates favoring laparoscopy (30-day rate: 3.3% vs. 5.9%, P=0.029; 90-day rate: 6.9% vs. 10.1%, P=0.018) (11). The other supposed advantages of laparoscopy were reduction of blood loss, shortened operative time, and reduction of length of hospital stays. At last, the quality of surgery was equal with similar conversion rates, similar number of resected lymph nodes, similar rates of R0 resection and equivalent long-term outcome compared to laparotomy (15).
Recently, the MIRO trial was published and provides a level-1 evidence on the benefits of hybrid laparoscopic Ivor Lewis over laparotomy (5). In this prospective and randomized trial, 104 patients were assigned to laparotomy and 103 to laparoscopy. The primary outcome was achieved with a significant reduction of the major postoperative morbidity in the 37 patients of the laparoscopy group (35.9%) compared to the 67 patients (64.4%) of the open group (OR 0.3; 95% CI: 0.1–0.5; P<0.001). One of the secondary outcomes achieved was the reduction of the pulmonary complications in the laparoscopy group: 18 patients (17%) compared to 31 patients (30%) in the open group (P=0.037). With a similar 30-day mortality (1.9% vs. 1.0%), the MIRO trial demonstrated similar oncological outcomes in term of number of resected LN and completeness of resection. Moreover, the long-term outcomes were similar between both approaches. Laparoscopy even demonstrated an unexpected better 5-year overall and disease-free survival rates compared to laparotomy. In an ancillary study, the MIRO trial further demonstrated that laparoscopy has a beneficial effect of health-related quality of life compared to laparotomy. This prevailed mostly for pain, social and role functioning with persistent differences up to 24 months after surgery. These benefits can be attributable to the reduction of postoperative complications in the laparoscopy group (21).
Main results of MIRO trial are provided in Table 1. The short-term outcomes were given in confrontation with the results of the randomized TIME trial displaying the comparison of total MIE with open approaches (4,5). Even if the two trials are not comparable in term of methodology and primary end-points, the question that remains is if the maximal benefit of a total MIE is in the abdominal or thoracic stage? The two trials resulted, with an equivalent magnitude, in a beneficial reduction on respiratory complications in the experimental group compared to conventional open techniques. The reduction seems to be however superior in TIME trial (RR: 0.35; 0.16–0.78) compared to MIRO trial (RR: 0.5; 0.26–0.96) but the numbers of patients included in the trial are different. As no surprise, MIRO trial demonstrated lower conversion rate compared to TIME trial because in MIRO trial one the two approaches was an open procedure. However, MIRO trial indicated a lower rate for reoperation requirement, suggesting less technical difficulties, which may likely revolve around the confection of the anastomosis. The oncological outcomes between the two trials seem equivalent. However, the control group of TIME trial demonstrated an unexpected high rate of incomplete resection compared to experimental group suggesting some bias in the inclusion protocol. At last, the long-term outcomes of both techniques have been reported and indicated a better survival in both experimental groups. In TIME trial, the 3-year overall survival rates were 40% in open group compared to 50% in MIE group. In MIRO trial, the 3- and 5-year overall survival rates were respectively 55% and 39% in open group and 67% and 60% in hybrid group. Out of TIME trial, two others retrospective studies have compared hybrid Ivor Lewis esophagectomy to total MIE (22,23). The conclusions of both studies did not find any evident superiority for one of the two techniques.
Table 1
| Clinical variables | TIME trial (total MIE) | MIRO trial (hybrid Ivor Lewis) | |||
|---|---|---|---|---|---|
| Open (N=56) | Total MIE (N=59) | Open (N=104) | Hybrid (N=103) | ||
| Operative time [min] | 299 | 329 | 330 | 327 | |
| Conversion [%] | – | 8 (14) | – | 3 (3) | |
| Pulmonary complications [%] | 19 [34] | 7 [12]* | 31 [30] | 18 [17]* | |
| Leakage [%] | 4 [7] | 7 [12] | 5 [5] | 8 [8] | |
| Reoperation [%] | 6 [11] | 8 [14] | 3 [3] | 2 [2] | |
| 30-day mortality [%] | 0 | 1 [2] | 2 [2] | 1 [1] | |
| Length of hospital stay (days) | 14 [1–120] | 11 [7–80] | 14 [7–95] | 14 [3–218] | |
| Number of resected LN [range] | 21 [7–47] | 20 [3–44] | 22 [9–64] | 21 [7–76] | |
| R0 resection [%] | 47 [84] | 54 [92] | 101 [98.1] | 97 [95.1] | |
| 3-year survival (%, 95% CI) | 40.4 [32–48] | 50.5 [42–58] | 55 [44–63] | 67 [57–75] | |
*, P<0.05. LN, lymph node.
On these bases and up till now, the conclusions that can be formulated are: whatever the techniques of MIE (hybrid or total), the use of a laparoscopy for the abdominal part of the esophagectomy demonstrates a strong benefit on postoperative respiratory outcomes without any compromise on oncological long-term outcomes. The laparoscopic approach should be seen as a new standard approach whatever the techniques used for the chest approach.
Hybrid esophagectomy including VATS
Data on results of hybrid esophagectomy including VATS associated to open laparotomy are scarce (1,9,10,24,25). The VATS techniques are heterogeneous including VATS Ivor Lewis with laparotomy and hybrid VATS McKeown esophagectomy. The VATS hybrid Ivor Lewis approach with performance of the anastomosis under thoracoscopy is not well reported due to the complexity of such procedures and the steep learning curve requiring at last 40 patients to be efficient. More details on the techniques of anastomosis are required for these procedures to be widespread worldwide with standardized and well-accepted methods. To date, there is at least 5 to 6 techniques described with in all huge results and outcomes (total mechanical, semi-automatic, circular, hand-sewn, transoral OrVil EEA, robotic) (26).
Conclusions
Hybrid esophagectomy is mostly represented by the laparoscopic hybrid Ivor Lewis esophagectomy. This technique appears safe, reproducible, and easy to teach without any modification of the technique of the intrathoracic anastomosis whereas total MIE requires to perform the anastomosis under thoracoscopy with disappointing results to date. This last point will be probably overcome in the near future by the standardization of the techniques of thoracoscopic anastomosis and the development of the robotic surgery.
The MIRO trial has provided good evidences that the unique use of laparoscopy for the abdominal stage of the esophagectomy resulted in a strong benefit on postoperative respiratory outcomes with the same magnitude to those observed with total MIE. This suggests that the maximum benefits of minimally invasive techniques are more provided by laparoscopy rather than thoracoscopy. Moreover the laparoscopy provides an excellent quality of dissection without any compromise on oncological long-term outcomes. Whatever the technique of MIE, the laparoscopic approach has to be seen as a new standard approach and should be incorporated to all esophageal cancer resections whenever possible. The results of the ROMIO study will clarify the benefit of addition of the thoracoscopy and to consider total MIE as a new standard (27).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Christopher R. Morse and Uma M. Sachdeva) for the series “Minimally Invasive Esophagectomy” published in Annals of Esophagus. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoe.2019.12.01). The series “Minimally Invasive Esophagectomy” was commissioned by the editorial office without any funding or sponsorship. XBD serves as an unpaid editorial board member of Annals of Esophagus from Oct. 2019 to Sep. 2021. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Decker G, Coosemans W, De Leyn P, et al. Minimally invasive esophagectomy for cancer. Eur J Cardiothorac Surg 2009;35:13-20. [Crossref] [PubMed]
- Bonavina L, Asti E, Sironi A, et al. Hybrid and total minimally invasive esophagectomy: how I do it. J Thorac Dis 2017;9:S761-72. [Crossref] [PubMed]
- van der Sluis PC, Schizas D, Liakakos T, et al. Minimally Invasive esophagectomy. Dig Surg 2019; [Crossref] [PubMed]
- Biere SS, van Berge Henegouwen MI, Maas KW, et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 2012;379:1887-92. [Crossref] [PubMed]
- Mariette C, Markar SR, Dabakuyo-Yonli TS, et al. Hybrid Minimally Invasive Esophagectomy for Esophageal Cancer. N Engl J Med 2019;380:152-62. [Crossref] [PubMed]
- van der Sluis PC, van der Horst S, May AM, et al. Robot-assisted Minimally Invasive Thoracolaparoscopic Esophagectomy Versus Open Transthoracic Esophagectomy for Resectable Esophageal Cancer: A Randomized Controlled Trial. Ann Surg 2019;269:621-30. [Crossref] [PubMed]
- Briez N, Piessen G, Torres F, et al. Effects of hybrid minimally invasive oesophagectomy on major postoperative pulmonary complications. Br J Surg 2012;99:1547-53. [Crossref] [PubMed]
- Voron T, Lintis A, Piessen G. Hybrid esophagectomy. J Thorac Dis 2019;11:S723-7. [Crossref] [PubMed]
- Cuschieri A, Shimi S, Banting S. Endoscopic oesophagectomy through a right thoracoscopic approach. J R Coll Surg Edinb 1992;37:7-11. [PubMed]
- Gossot D, Fourquier P, Celerier M. Thoracoscopic esophagectomy: technique and initial results. Ann Thorac Surg 1993;56:667-70. [Crossref] [PubMed]
- Messager M, Pasquer A, Duhamel A, et al. Laparoscopic gastric mobilization reduces postoperative mortality after esophageal cancer surgery: A French Nationwide Study. Ann Surg 2015;262:817-22; discussion 822-3. [Crossref] [PubMed]
- Bjelovic M, Babic T, Spica B, et al. Could hybrid minimally invasive esophagectomy improve the treatment results of esophageal cancer? Eur J Surg Oncol 2016;42:1196-201. [Crossref] [PubMed]
- Yun JS, Na KJ, Song SY, et al. Comparison of perioperative outcomes following hybrid minimally invasive versus open Ivor Lewis esophagectomy for esophageal cancer. J Thorac Dis 2017;9:3097-104. [Crossref] [PubMed]
- Glatz T, Marjanovic G, Kulemann B, et al. Hybrid minimally invasive esophagectomy vs. open esophagectomy: a matched case analysis in 120 patients. Langenbecks Arch Surg 2017;402:323-31. [Crossref] [PubMed]
- Rinieri P, Ouattara M, Brioude G, et al. Long-term outcome of open versus hybrid minimally invasive Ivor Lewis oesophagectomy: a propensity score matched study†. Eur J Cardiothorac Surg 2017;51:223-9. [PubMed]
- Simonneau G, Vivien A, Sartene R, et al. Diaphragm dysfunction induced by upper abdominal surgery. Role of postoperative pain. Am Rev Respir Dis 1983;128:899-903. [PubMed]
- Ford GT, Whitelaw WA, Rosenal TW, et al. Diaphragm function after upper abdominal surgery in humans. Am Rev Respir Dis 1983;127:431-6. [Crossref] [PubMed]
- Coelho JC, de Araujo RP, Marchesini JB, et al. Pulmonary function after cholecystectomy performed through Kocher’s incision, a mini-incision, and laparoscopy. World J Surg 1993;17:544-6. [Crossref] [PubMed]
- Frazee RC, Roberts JW, Okeson GC, et al. Open versus laparoscopic cholecystectomy. A comparison of postoperative pulmonary function. Ann Surg 1991;213:651-3. [Crossref] [PubMed]
- Degisors S, Pasquer A, Renaud F, et al. Are Thoracotomy and/or Intrathoracic Anastomosis Still Predictors of Postoperative Mortality After Esophageal Cancer surgery?: A Nationwide Study. Ann Surg 2017;266:854-62. [Crossref] [PubMed]
- Mariette C, Markar S, Dabakuyo-Yonli TS, et al. Health-related Quality of Life Following Hybrid Minimally Invasive Versus Open Esophagectomy for Patients With Esophageal Cancer, Analysis of a Multicenter, Open-label, Randomized Phase III Controlled Trial: The MIRO Trial. Ann Surg 2019; [Crossref] [PubMed]
- Bonavina L, Scolari F, Aiolfi A, et al. Early outcome of thoracoscopic and hybrid esophagectomy: Propensitymatched comparative analysis. Surgery 2016;159:1073-81. [Crossref] [PubMed]
- Berlth F, Plum PS, Chon SH, et al. Total minimally invasive esophagectomy for esophageal adenocarcinoma reduces postoperative pain and pneumonia compared to hybrid esophagectomy. Surg Endosc 2018;32:4957-65. [Crossref] [PubMed]
- Law S, Fok M, Chu KM, et al. Thoracoscopic esophagectomy for esophageal cancer. Surgery 1997;122:8-14. [Crossref] [PubMed]
- Liu HP, Chang CH, Lin PJ, et al. Video-assisted endoscopic esophagectomy with stapled intrathoracic esophagogastric anastomosis. World J Surg 1995;745-7. [Crossref] [PubMed]
- Maas KW, Biere SS, Scheepers JJ, et al. Minimally invasive intrathoracic anastomosis after Ivor Lewis esophagectomy for cancer: a review of transoral or transthoracic use of staplers. Surg Endosc 2012;26:1795-802. [Crossref] [PubMed]
- Avery KN, Metcalfe C, Berrisford R, et al. The feasibility of a randomized controlled trial of esophagectomy for esophageal cancer--the ROMIO (Randomized Oesophagectomy: Minimally Invasive or Open) study: protocol for a randomized controlled trial. Trials 2014;15:200. [Crossref] [PubMed]
Cite this article as: Fourdrain A, Thomas PA, D’Journo XB. Hybrid approaches to minimally invasive esophagectomy. Ann Esophagus 2019;2:20.


