
Distended neoesophagus in a man with congenital esophageal atresia
Introduction
A few cases have been reported requiring revision surgery more than 20 years after colonic interposition for congenital esophageal atresia. Revision surgery may relieve symptoms and improve quality of life. Further reconstructive options may be limited due to the lack of an available conduit (1). Here we report an interesting case with sequelae of esophageal reconstruction requiring complete preoperative evaluation and delicate revision surgery.
Case presentation
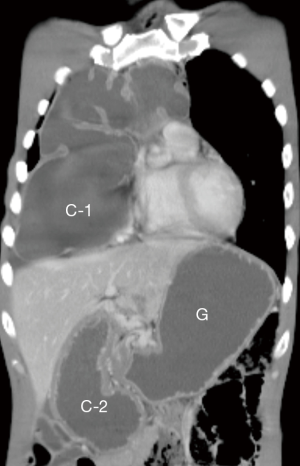
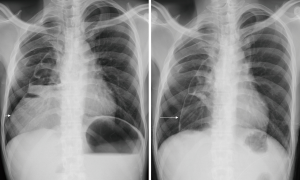
A 33-year-old married man presented with abdominal fullness and chest tightness. He was diagnosed as congenital esophageal atresia a few days after birth. The young man had undergone a total of 6 times of surgeries to solve the problem of congenital esophageal atresia at a medical center in northern Taiwan. In the newborn period, he underwent division of tracheoesophageal fistula, cervical esophagostomy, and gastrostomy. Subsequently, esophageal reconstruction was performed using ileocolon via retrosternum at age of 2. In recent 2 years, he had intermittent abdominal pain, abdominal fullness, and chest tightness, and lost 5 kg of body weight. Chest film showed marked dilatation of the neoesophagus with compression of right lung. Endoscopy showed stenosis of colon-gastrostomy. He searched our thoracic service for revision surgery. His body height was 169.8 cm, and body weight was 49.3 kg. Physically, the abdominal wall presented with irregular wound scar that related to previous wound infection. Laboratory data were all within normal limits. Computed tomography (Figure 1) revealed a distended neoesophagus (C-1) extended to abdominal cavity (C-2) and gastric dilatation (G). According to the preoperative evaluation, some sequelae of esophageal reconstruction were considered such as narrowing of colon-gastrostomy, subxiphoid compression of neoesophagus, redundancy of neoesophagus, and severe intestinal adhesion. To solve these problems, he underwent laparotomy with enterolysis, release of subxiphoid compression, revision of cologastrostomy (A1), and creation of colojejunostomy (A2) (Figure 2). At surgery, partial obstruction of the pylorus was detected by endoscopy and severe intestinal adhesion was confirmed. Following the revision surgery, chest films (Figure 3) showed the distended neoesophagus (left) yielded shrinking (right). Patient could drink water on postoperative day 10 and liquid diet on postoperative day 12. He was discharged on postoperative day 14 after examination of upper gastrointestinal series. He resumed regular diet on postoperative day 16 and was well in the out-patient-clinic follow-up.
Comments
In our experience of esophageal reconstruction, the common use of the esophageal substitute was ileocolon. Obstruction or redundancy of the neoesophagus was very rare (2). We have reported 14 cases requiring surgical revision for proximal anastomotic strictures after hypopharyngocolostomy or esophagocolostomy. These proximal strictures can be surgically corrected after excision of the scar and mobilization of the esophageal substitute through a cervical incision only or a cervical incision plus sternotomy (3). Some researchers reported a few patients requiring reoperation for late obstruction due to volvulus or kinking because of redundancy (4). Comparing to the proximal anastomotic stenosis, occurrence of the distal anastomotic stenosis is rare. Primary direct anastomosis is feasible in patients with congenital esophageal atresia with tracheoesophageal fistula. However, in case of without tracheoesophageal fistula required esophageal reconstruction because esophageal long gap (5). In the present case, he underwent 6 times of surgeries including esophageal reconstruction in the infancy because of unsuccessful primary anastomosis. Some authors emphasized that long-term follow-up of patients who underwent esophageal replacement in children is essential because of gradual changes in the function of the graft, strictures at the anastomosis and the unknown risks of Barrett’s esophagus (6). We kept this patient in the hospital until post-operative day 14 because we were concerned about the operative finding of intestinal adhesion.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoe.2018.10.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dhir R, Sutcliffe RP, Rohatgi A, et al. Surgical management of late complications after colonic interposition for esophageal atresia. Ann Thorac Surg 2008;86:1965-7. [Crossref] [PubMed]
- Wu MH, Tseng YT, Lin MY, et al. Esophageal reconstruction for hypopharyngoesophageal strictures after corrosive injury. Eur J Cardiothorac Surg 2001;19:400-5. [Crossref] [PubMed]
- Wu MH, Lai WW, Lin MY, et al. Prevention and management of strictures after hypopharyngocolostomy or esophagocolostomy. Ann Thorac Surg 1994;58:108-11. [Crossref] [PubMed]
- Sterling RP, Kuykendall RC, Carmichael MJ, et al. Unusual sequelae of colon interposition for esophageal reconstruction: late obstruction requiring reoperation. Ann Thorac Surg 1984;38:292-5. [Crossref] [PubMed]
- Wu MH. Primary repair and correction of anastomotic stenosis in congenital esophageal atresia. Formosan J Surg 2003;36:120-4.
- Arul GS, Parikh D. Oesophageal replacement in children. Ann R Coll Surg Engl 2008;90:7-12. [Crossref] [PubMed]
Cite this article as: Wu MH, Wu HY. Distended neoesophagus in a man with congenital esophageal atresia. Ann Esophagus 2018;1:16.



